ORIF - Plate fixation
1. General considerations
Introduction
Plating with precontoured periarticular locking plates provides angular-stable fixation and is the most commonly used method of distal humeral fracture fixation.
Treatment principle
If the articular fracture is stable when reduced, it may be stabilized by interfragmentary compression (usually during plate application).
If there is comminution in the central region between the trochlea and capitellum and the articular block is not stable after reduction, interfragmentary compression will not be indicated. Reconstruction of the medial trochlear ridge and lateral column is prioritized.
If one column has a simple fracture (ie, intrinsic stability after reduction), it is stabilized first with interfragmentary compression.
The other column has a comminuted fracture (simple or fragmentary wedge) which has no intrinsic stability after reduction. This is stabilized next by bridge plating.
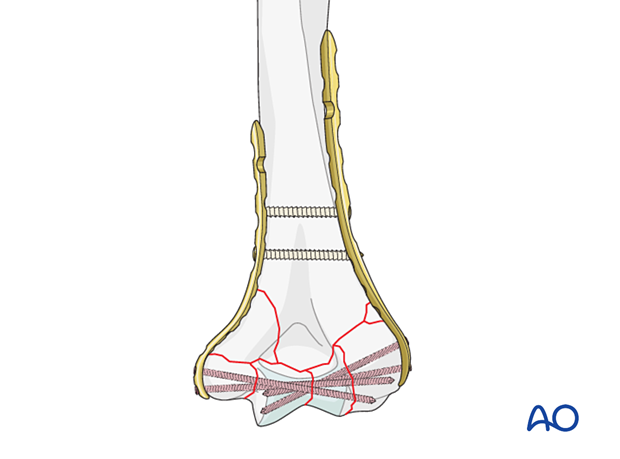
If both columns have comminuted fractures, then both are stabilized by bridge plating
For many comminuted fractures, it is preferable to bridge the comminution without reducing and securing each fragment individually.
This approach preserves the blood supply and healing capacity of the fragments while relying on the implants for relative stability until early healing is established.
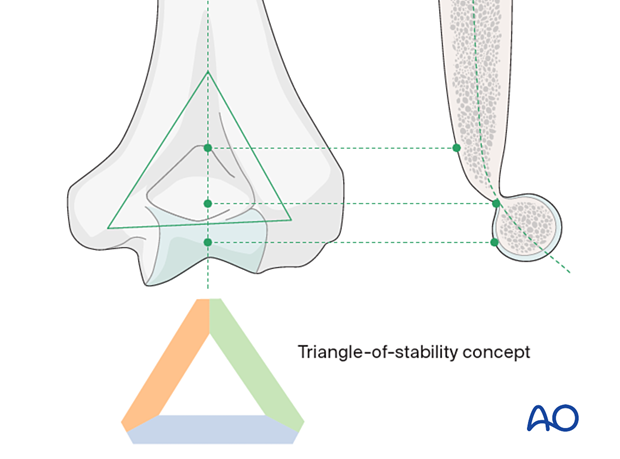
Triangle-of-stability concept
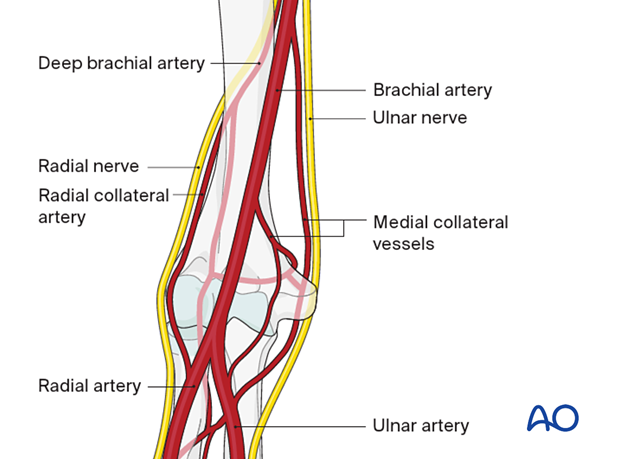
The mechanical properties of the distal humerus are based on a triangle of stability, comprising the medial and lateral columns and the articular block (see also the anatomical concepts).
In principle, the intraarticular fracture is fixed first. Thereby the fracture is converted to an extraarticular fracture and treated likewise. The less complex column is then addressed next.
Parallel vs perpendicular plating
There is little biomechanical evidence from in vitro studies to suggest that one has more advantages than the other. However, in clinical practice, a specific fracture pattern may indicate a specific plate construct.
In a very low transverse fracture, ie, exiting at or below the level of the olecranon fossa, the articular block does not provide enough hold for the application of a dorsolateral plate.
An alternative is a dorsolateral plate with lateral tab. This permits insertion of screws from lateral-to-medial into the articular block as well as posterior-to-anterior into the capitellum.
Plate selection
Precontoured anatomical plates have been designed. If these are not available, at least one column (usually the lateral column) should be fixed with a small-fragment LCP in bridging mode. The other column can also be fixed with a small-fragment LCP or a reconstruction plate in bridging mode.
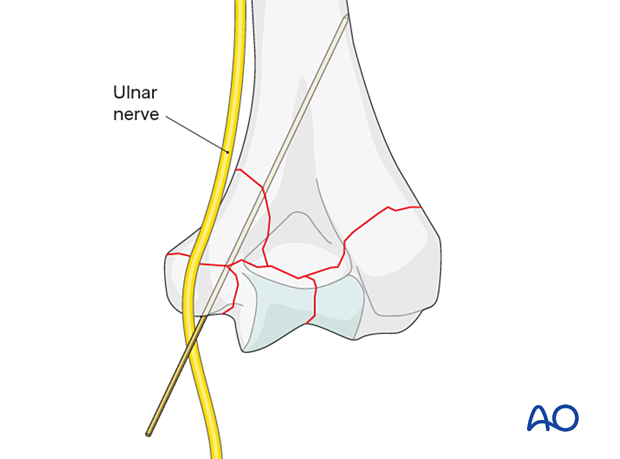
Note: ulnar nerve at risk
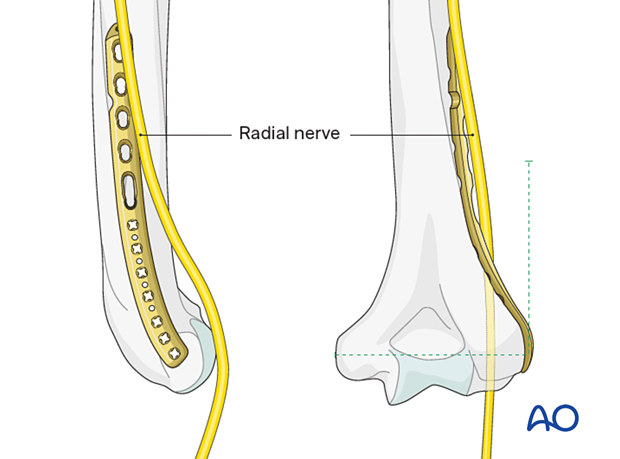
Note: radial nerve at risk
2. Patient preparation and approaches
Patient positioning
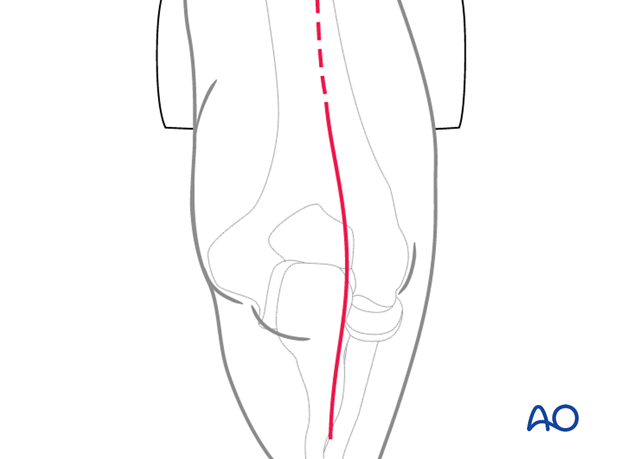
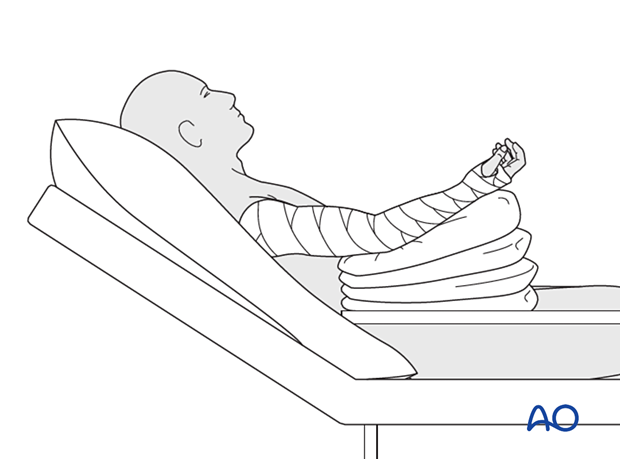
This procedure is usually performed with the patient either in a prone position or lateral decubitus position.
Approaches
A posterior triceps-elevating approach is preferred. However, triceps-on or olecranon osteotomy approaches may be used depending on surgeon’s preference.
The triceps-split approach does not allow for accurate control of the articular block and column fixation and is therefore not recommended.
3. Preparing the fracture site
In principle, preserve all fracture fragments attached to soft tissue in situ if possible.
Keep removal of hematoma to the minimum necessary to facilitate the exposure of the fracture.
4. Reduction and fixation of articular block
Indirect reduction
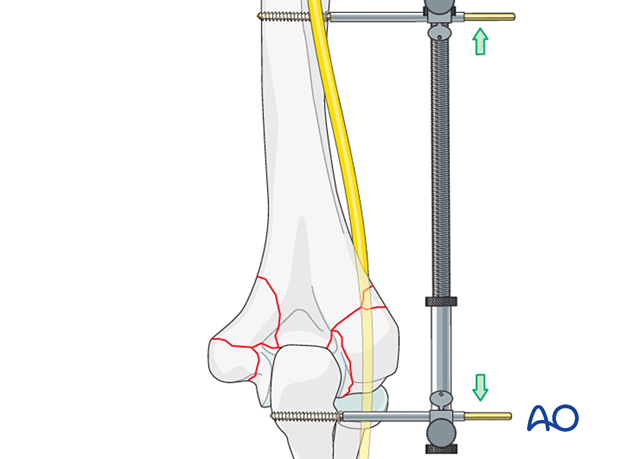
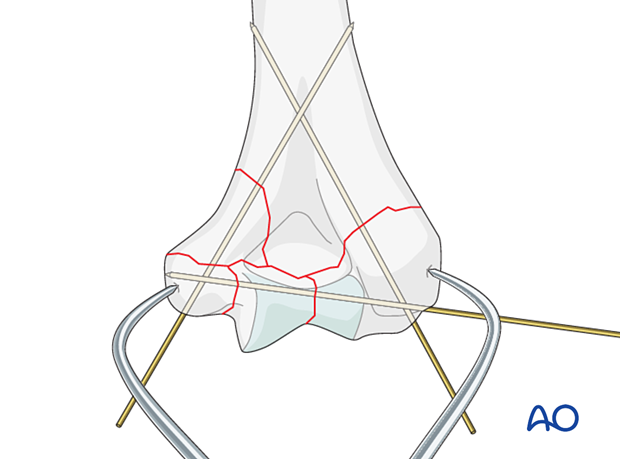
In case of comminution of both columns, an external fixator or distractor may be used to provisionally control angular and rotational alignment, although in most cases, manual traction is sufficient.
Distraction may be performed by transarticular or periarticular pin placement depending on the available bone stock of the articular segment.
Articular reduction
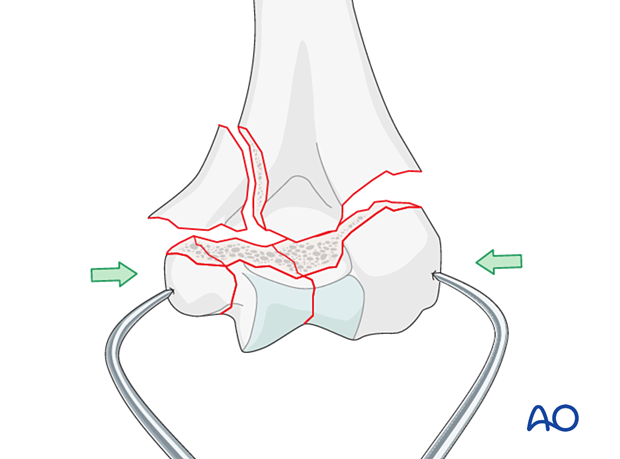
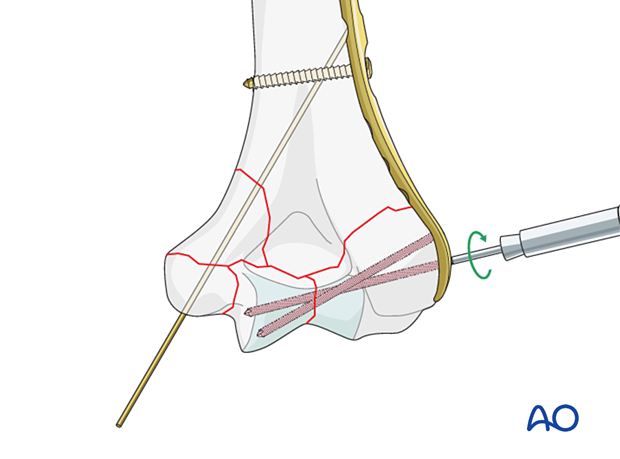
Reduce the articular fragments manually, with K-wire joysticks or pointed reduction forceps.
Hold the reduced articular block with pointed reduction forceps. Thereby extrinsic interfragmentary compression is gained.
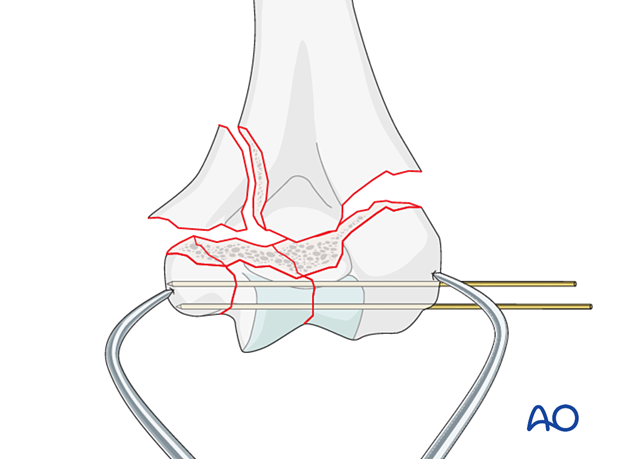
Temporarily fix the fragments with K-wires.
With a K-wire, interfragmentary positioning is achieved but no compression.
Pitfall: overcompression
Option: position screw(s)
In poor-quality bone or multifragmentary fractures, interfragmentary compression is undesirable, and therefore interfragmentary alignment is gained with a position screw.
Positioning screws through a locking plate are preferred. If desired or locking plates are not available, these screws may be inserted outside a plate.
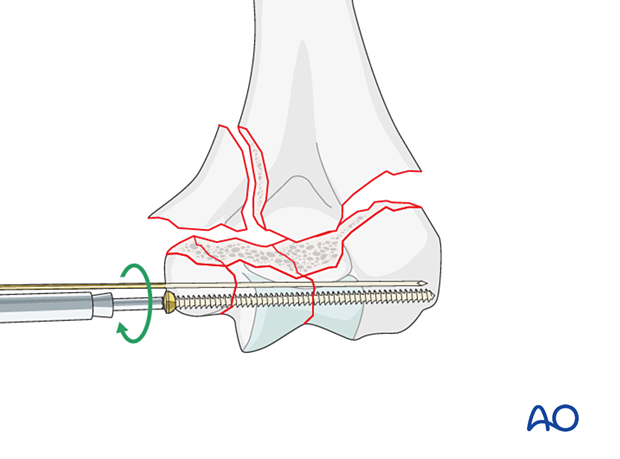
In very distal fractures, the positioning K-wire can be retained to maintain rotational stability.
5. Supracondylar reduction and fixation
Basic techniques
The basic technique for application of anatomical plates is described in:
If precontoured anatomical plates are not available, see the basic technique for application of reconstruction plates.
Reduction and temporary fixation
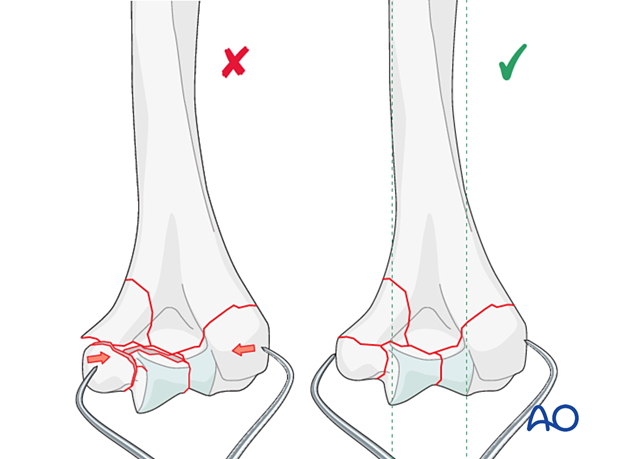
Reduce the reconstituted articular (condylar) block to the more stable column and use one or more K-wires for preliminary fixation.
Reduce the comminuted fragment of the other column into correct alignment and use one or more K-wires for preliminary fixation.
Ensure an accurate alignment of the articular block to the shaft (see also the anatomical concepts).
It is recommended to check alignment under image intensification.
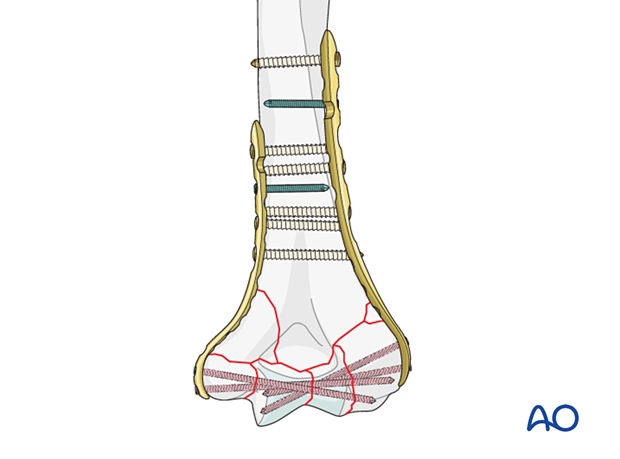
Application of the first plate
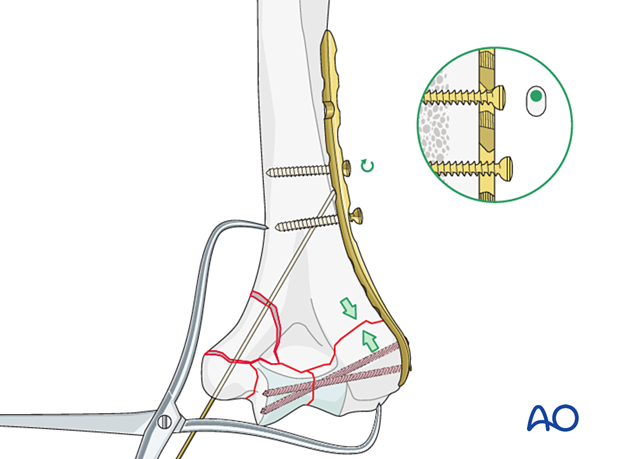
Apply the first plate to the less fragmented column.
Provisionally fix the plate to the bone with a cortical position screw through a slotted combihole proximal to the fracture.
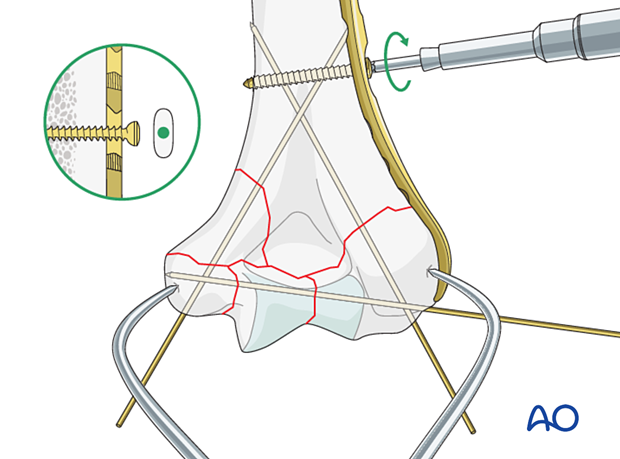
Place a locking screw through the plate into the articular block to hold the reduction. Make sure it is long enough to engage in the other condylar fragment. If possible, use two long locking screws.
Compression plating for simple column fracture
A column fracture with intrinsic stability after reduction may be fixed with compression plating.
Compression is applied to the simple column fracture before placement of the other plate.
Release the positioning screw slightly and insert a bicortical cortical screw eccentrically in a more proximal plate hole for compression in the plane of the plate. Then tighten the positioning screw.
Insert at least one further proximal cortical screw in neutral mode or a locking screw, usually in the most proximal screw hole.
The other, less stable column fracture may be fixed with bridge plating as described below.
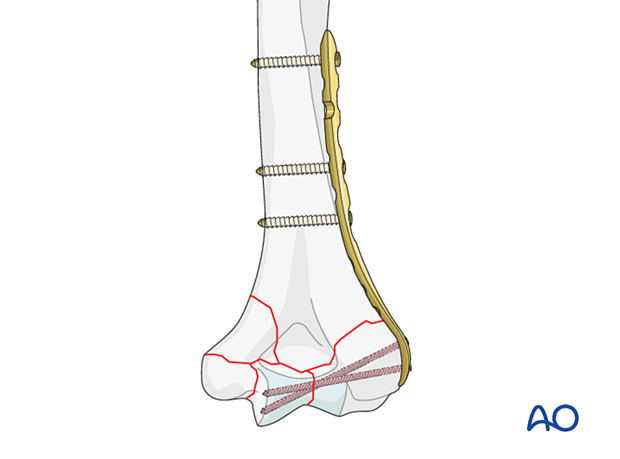
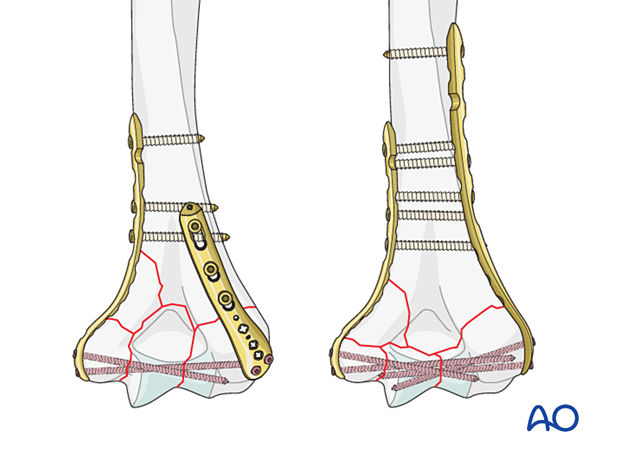
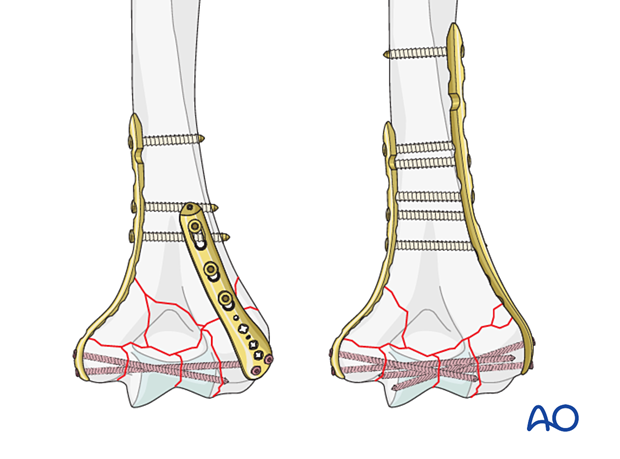
Bridge plating for comminuted column fractures
A comminuted column fracture with lack of intrinsic stability after reduction should be fixed with bridge plating.
If the columnar fragmentation is unstable, no compression should be exerted.
Before inserting further screws into the first plate, apply the second plate to the bone and provisionally fix it in the same way as the first.
Insert a long locking screw into the articular block, two if possible, engaging into the other condylar fragment.
Insert at least one further proximal screw in both columns. This can be either a cortical screw in the neutral mode or a locking screw, depending on bone quality.
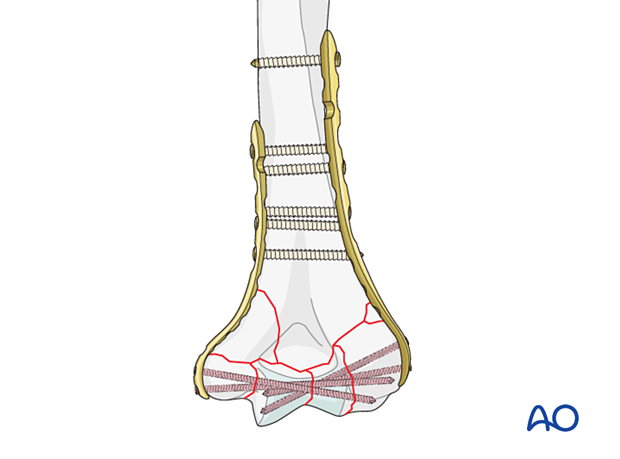
Insertion of remaining screws
In poor-quality bone, insert further locking screws in the diaphyseal segment.
The screw density should be similar on both columns.
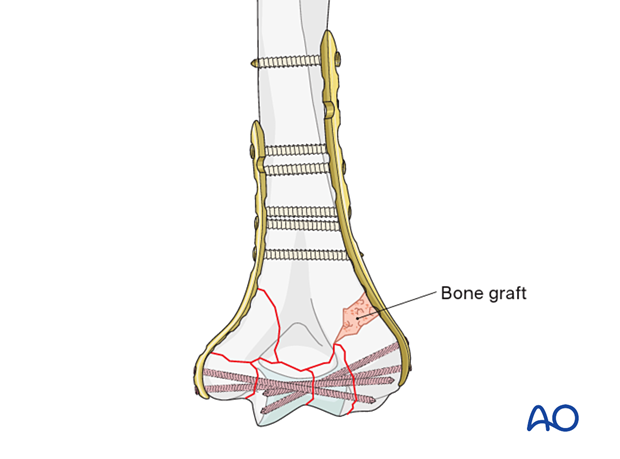
Bone graft
In case of great metaphyseal comminution, or missing bone, use a bone graft or the preserved fracture fragments.
Make sure not to graft the olecranon fossa.
6. Final assessment
Visually inspect the fixation and manually check for fracture stability.
Repeat the manual check under image intensification.
Ensure the ulnar nerve is not unstable or tethered on implants throughout a full range of motion.
7. Aftercare
Introduction
The rehabilitation protocol consists usually of three phases:
- Rehabilitation until wound healing
- Rehabilitation until bone healing
- Functional rehabilitation after bone healing
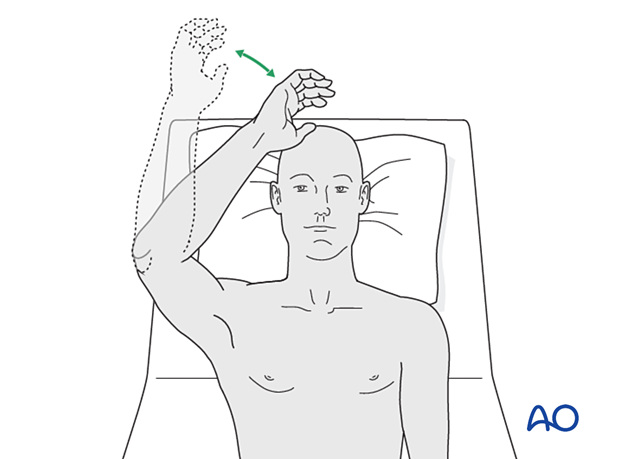
Immediate aftercare
The arm is bandaged to support and protect the surgical wound.
The arm is rested on pillows in slight flexion of the elbow so that the hand is positioned above the level of the heart.
Short-term splinting may be applied for soft-tissue support.
Neurovascular observations are made frequently.
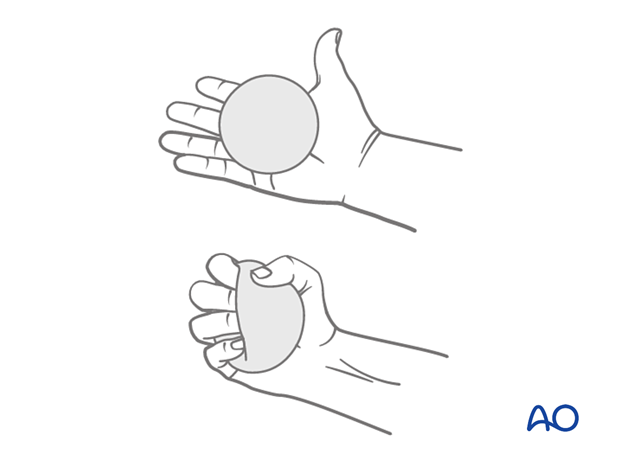
Hand pumping and forearm rotation exercises are started as soon as possible to reduce lymphedema and to improve venous return in the limb. This helps to reduce postoperative swelling.
Mobilization until wound healing
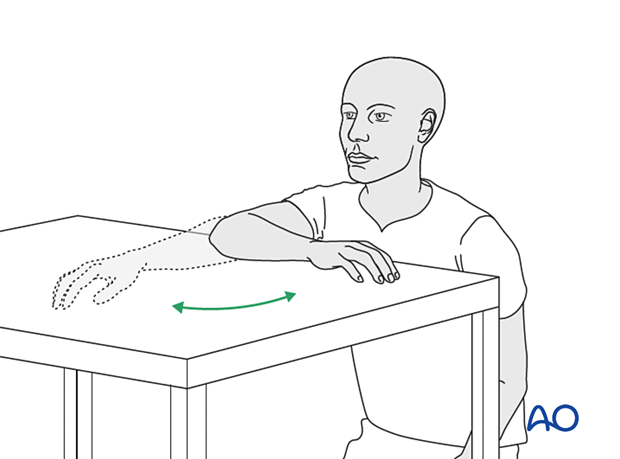
Gravity-eliminated active assisted exercises of the elbow should be initiated as soon as possible, as the elbow is prone to stiffness:
- The bandages are removed, and the arm rested on a side table
- Flexion/extension of the arm at the elbow is encouraged in a gentle sweeping movement on the tabletop as far as comfort permits (as illustrated)
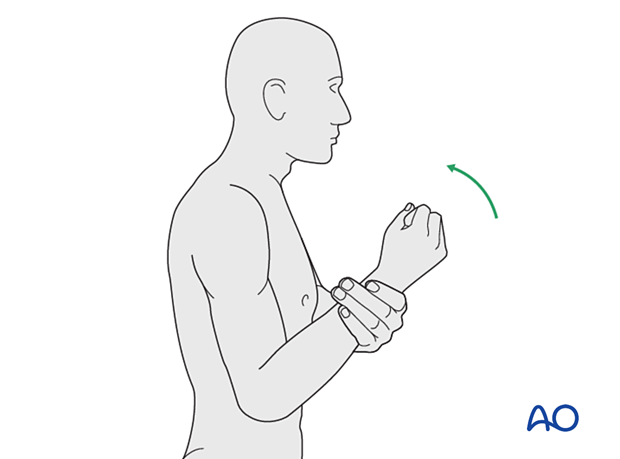
- Full pronation and supination in protected arm position is encouraged
- Exercises are performed hourly in repetitions, the number of which is governed by comfort
- Between periods of exercise, the elbow is rested in the elevated position for at least the first 48 hours postoperatively
- Keep the arm elevated between periods of exercise until the wound has healed
Rehabilitation until bone healing
Active patient-directed range-of -motion exercises should be encouraged without the routine use of splintage or immobilization.
Avoid forceful motion, repetitive loading, or weight-bearing through the arm.
A simple compressive sleeve can provide proprioceptive feedback which can help regain motion and avoid cocontraction.
No load-bearing (ie, pushing, pulling, or carrying weights) or strengthening exercises are allowed until early fracture healing is established by x-ray and clinical examination.
This is usually a minimum of 8–12 weeks after injury. Weight-bearing on the arm should be avoided until bony union is assured.
The patient should avoid resisted extension activities, especially after a triceps-elevating approach or olecranon osteotomy.
Rehabilitation after bone healing
When the fracture has united, a combination of active functional motion and kinetic chain rehabilitation can be initiated.
Active assisted elbow motion exercises are continued. The patient bends the elbow as much as possible using his/her muscles while simultaneously using the opposite arm to gently push the arm into further flexion. This effort should be sustained for several minutes; the longer, the better.
Next, a similar exercise is performed for extension.
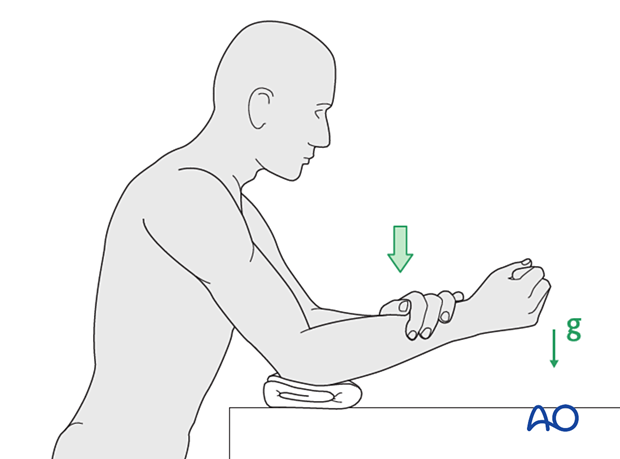
If the patient finds it difficult to accomplish these exercises when seated, then performing the same exercises when lying supine can be helpful.
Implant removal
Generally, the implants are not removed. If symptomatic, hardware removal may be considered after consolidated bony healing, usually no less than 6 months for metaphyseal fractures and 12 months when the diaphysis is involved. The avoidance of the risk of refracture requires activity limitation for some months after implant removal.
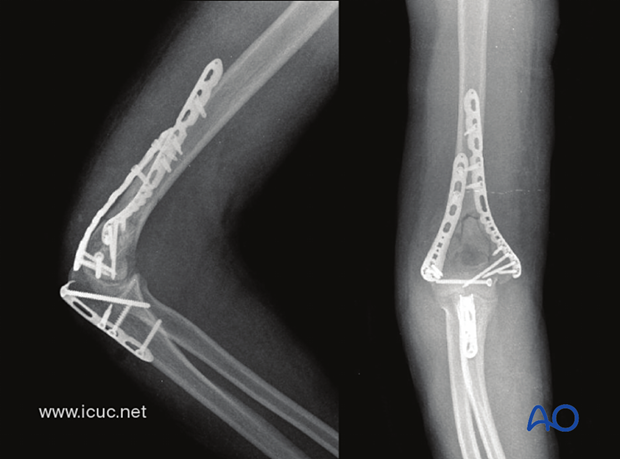
8. Case
3D-CT demonstrating a C-type distal humeral fracture with much comminution.

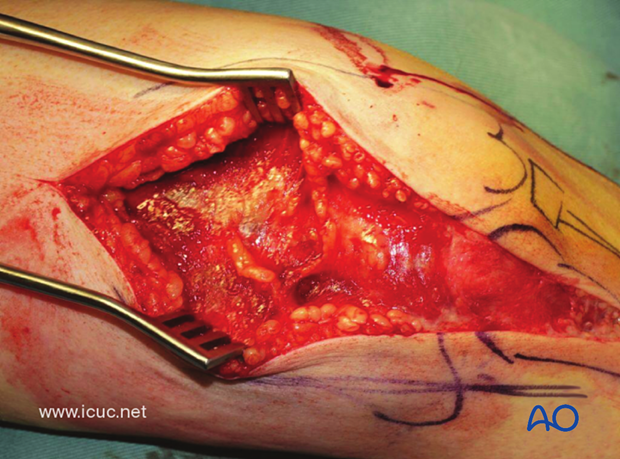
This image shows the patient with the arm hanging over a bolster in the operating room which allows for the best surgical approach to this difficult fracture.

The surgical anatomy has been drawn on the patient's elbow and a small, lateral, grade 1 open wound is present.

This is a complex, intraarticular fracture. Anatomic reduction is required to give the best functional outcome. This requires adequate exposure.
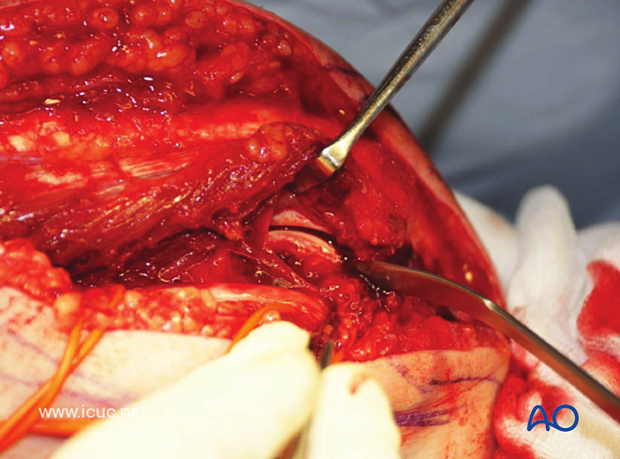
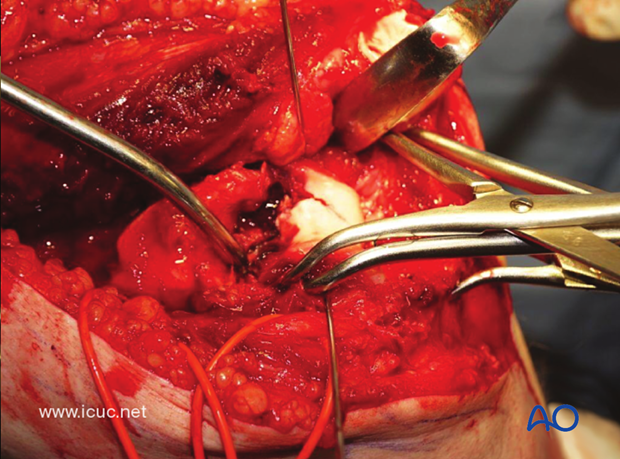
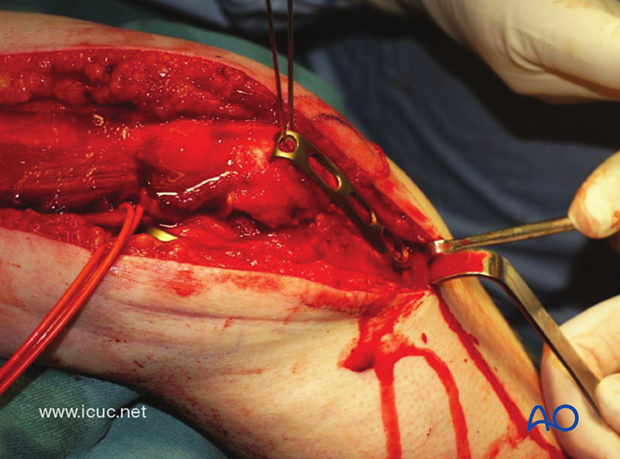
The ulnar nerve is carefully dissected and protected on the medial side.
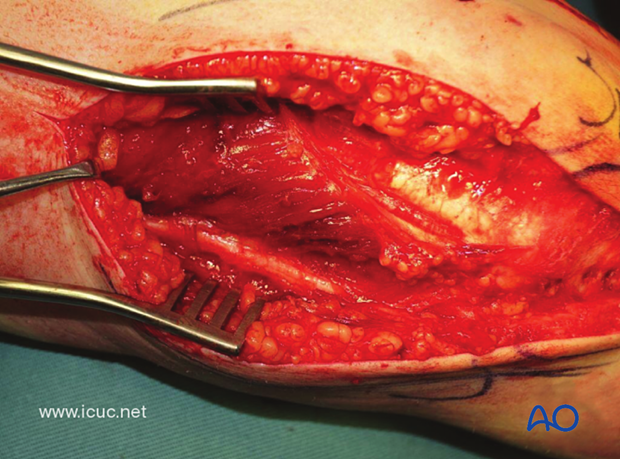
This image shows a carefully dissected and protected branch to the flexor carpi ulnaris.
By dissecting medially from the cubital tunnel, the bare spot of the olecranon can be found. This is the best spot for the osteotomy of the olecranon.
A Chevron osteotomy is carefully started with a saw, but not completed.
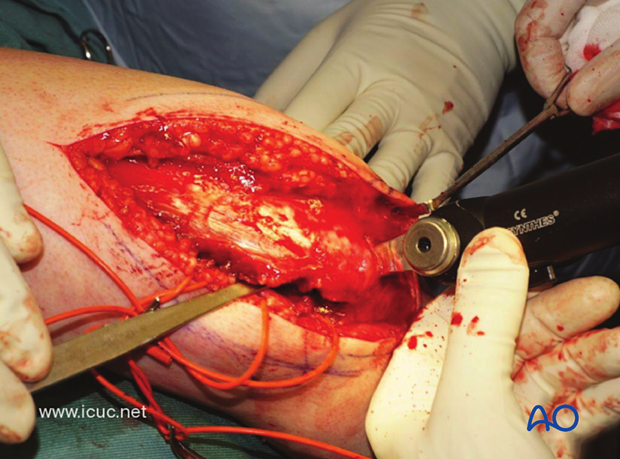
The olecranon osteotomy is completed with an osteotome.
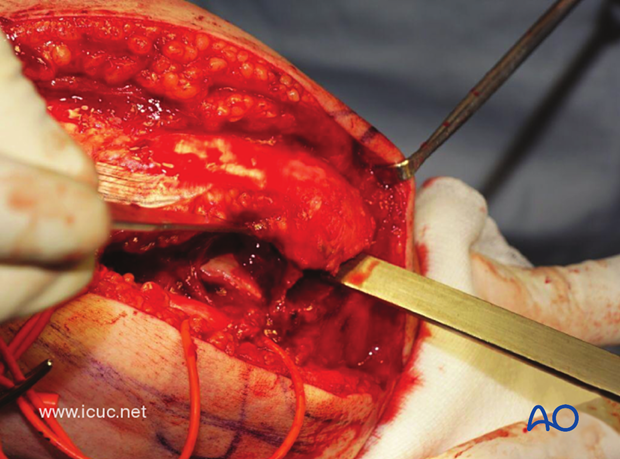
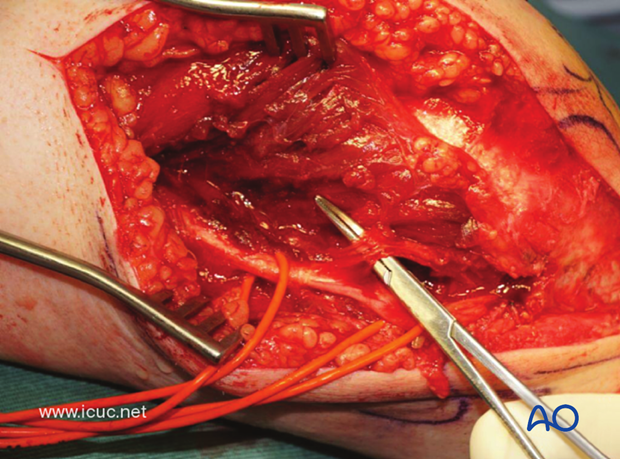
The olecranon osteotomy, when completed, reveals a badly comminuted C3 distal humeral fracture.
Often small cortical pieces are found without soft tissue attachment and are discarded.
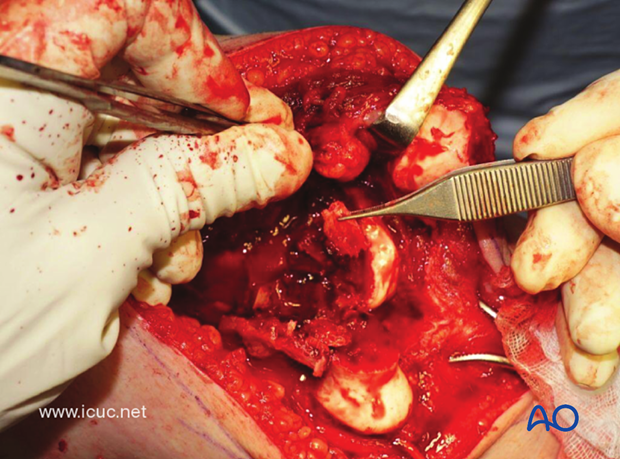
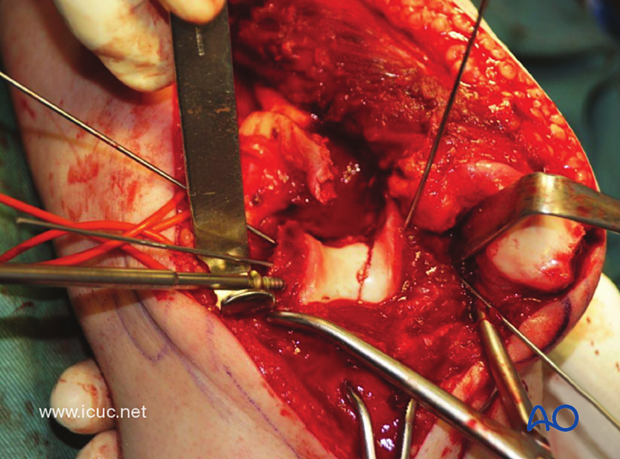
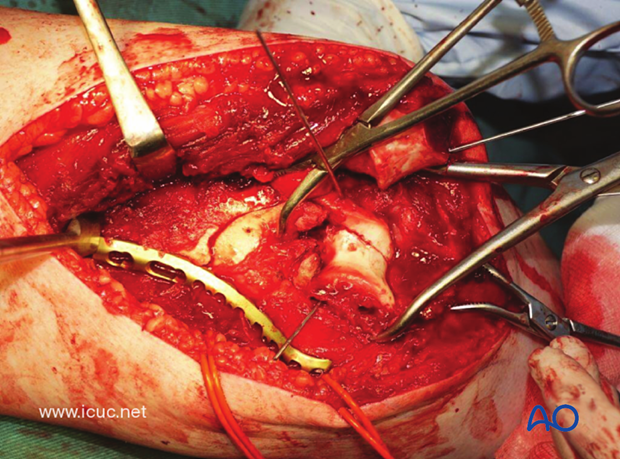
The surgical tactic is started by reducing the articular components, converting the C-type fracture into an A-type fracture.
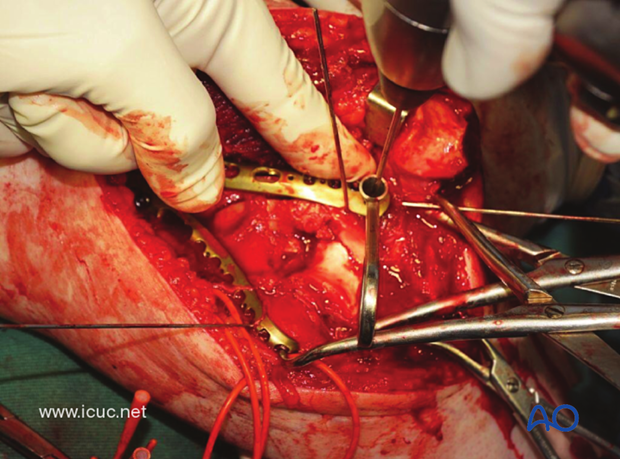
The joint is carefully reduced and held with a temporary K-wire. Note the ulnar nerve is carefully protected. K-wires are being used as joysticks.
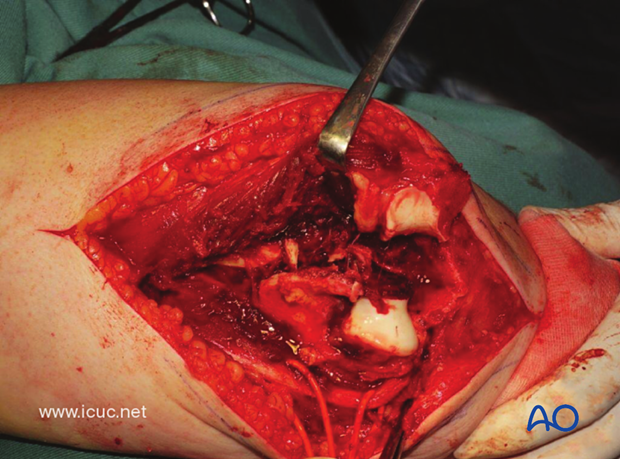
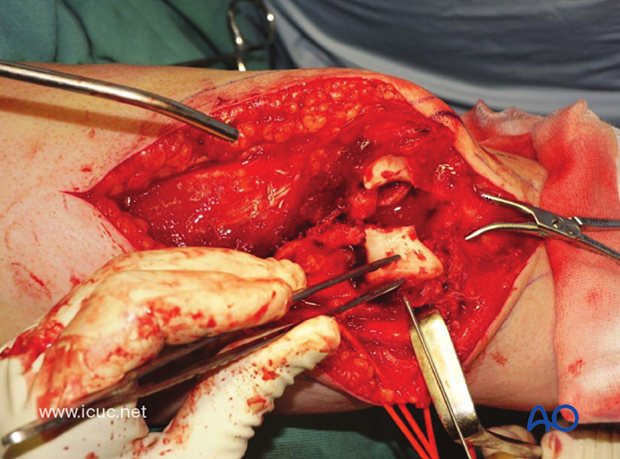
Sometimes the joint surface has missing fragments, which makes reconstruction difficult. However, the width, length, and depth of the condylar region must be maintained as it articulates with the olecranon and radial head.
This intraoperative video demonstrates the joint reduction and the significant metaphyseal comminution.
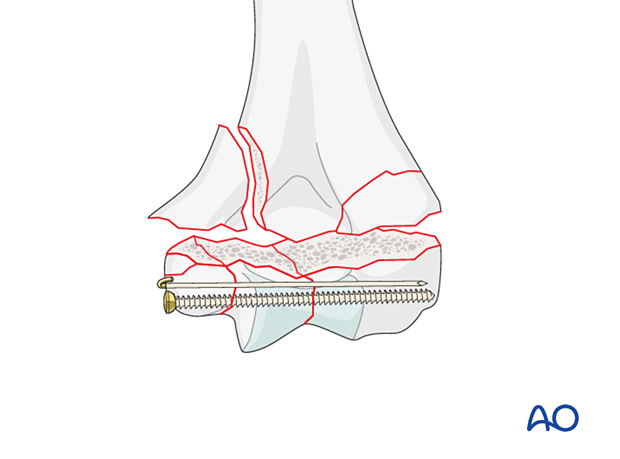
The carefully reconstructed joint surface is held nicely with a transcondylar lag screw.
The medial VA LCP must be carefully placed beneath the mobile ulnar nerve.
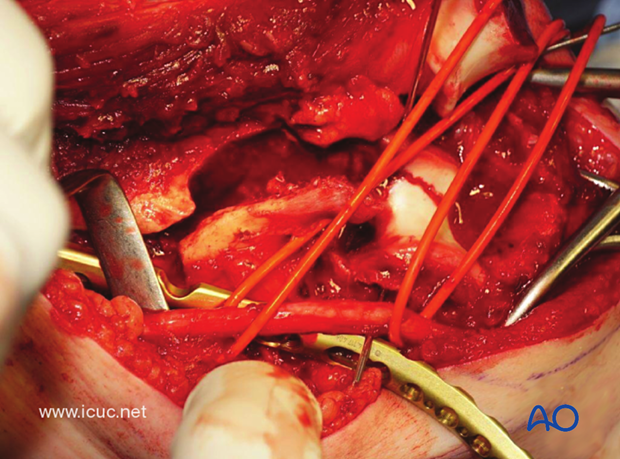
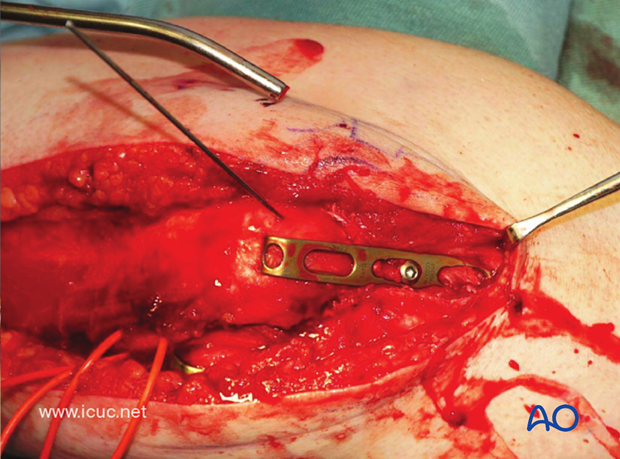
The medial LCP may be used as a reduction plate with locking screws distally assisting with transcondylar fixation.
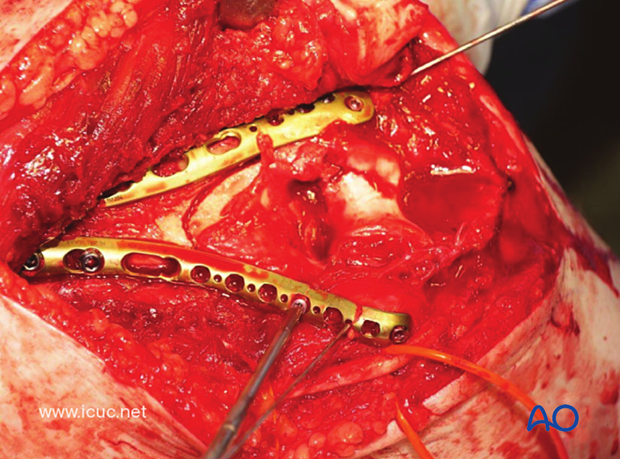
With the medial plate applied, the metaphyseal comminution is bridged temporarily.
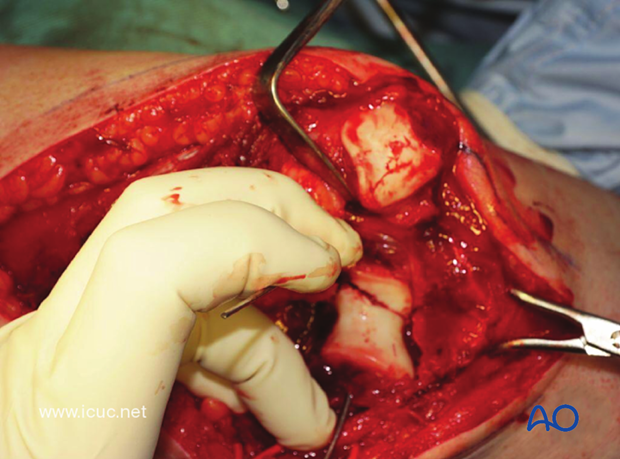
Once the metaphyseal component is reduced, proximal fixation can be performed.
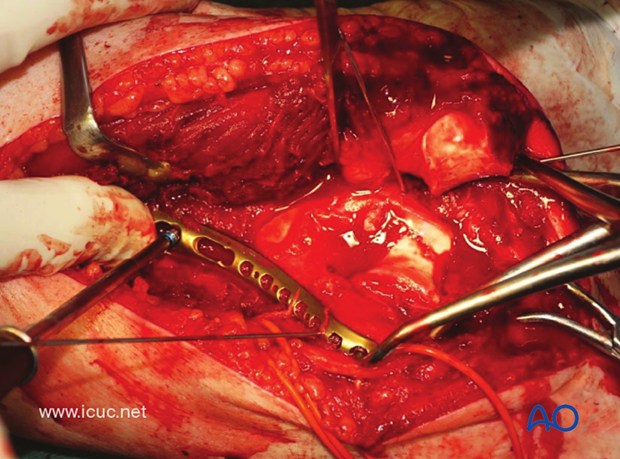
A posterolateral LCP can then be applied as a reduction plate to supplement the medial fixation.
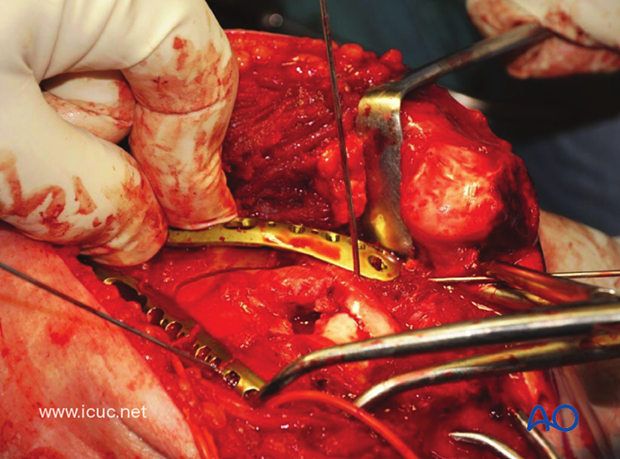
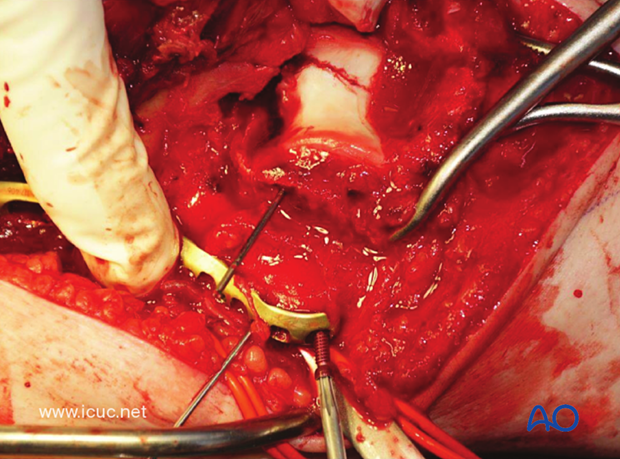
Great care must be taken to ensure that the distal end of the lateral plate is clear of the olecranon fossa, so as not to compromise extension of the elbow.
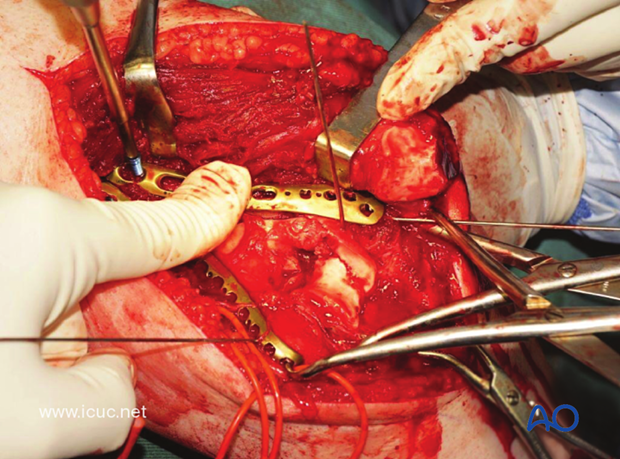
The variable angle lateral plate should obtain at least 3 points of distal fixation. Care must be taken when placing these screws to avoid penetrating the radio capitellar joint.
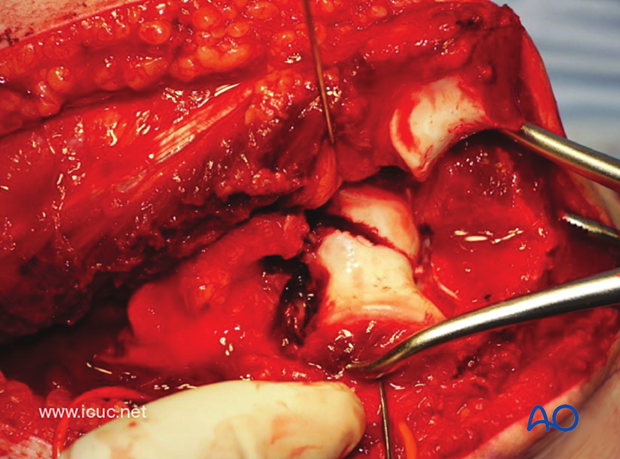
Once the two plates are fixed proximally and distally, further screws may be inserted, but the principle of bridging the comminuted fracture is maintained.
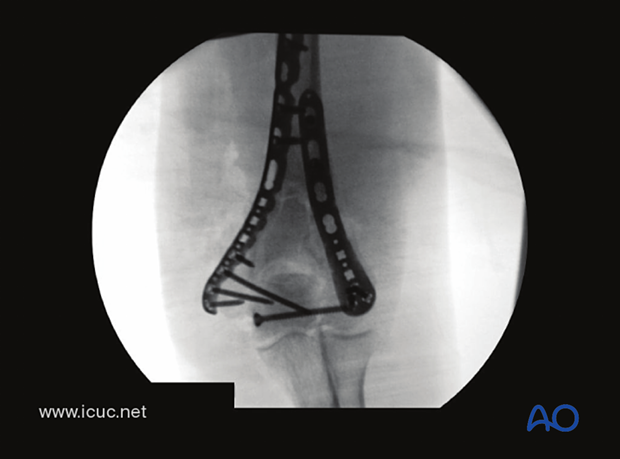
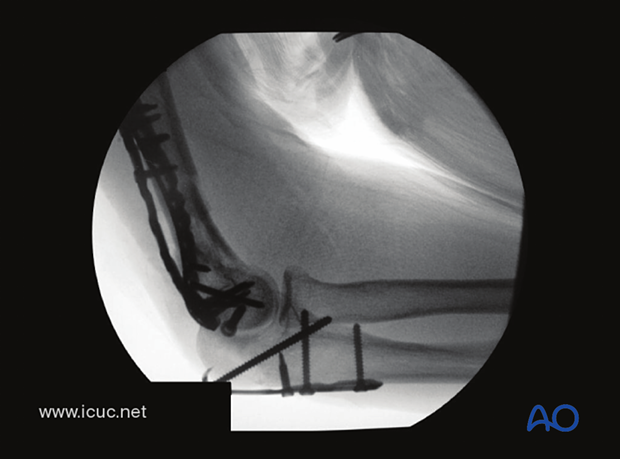
AP X-ray demonstrates the lag screw reducing the articular fracture and nice, two-sided, stable fixation. Note the fixation is bridging the metaphyseal fragments.
The Chevron osteotomy is closed and held with K-wires.
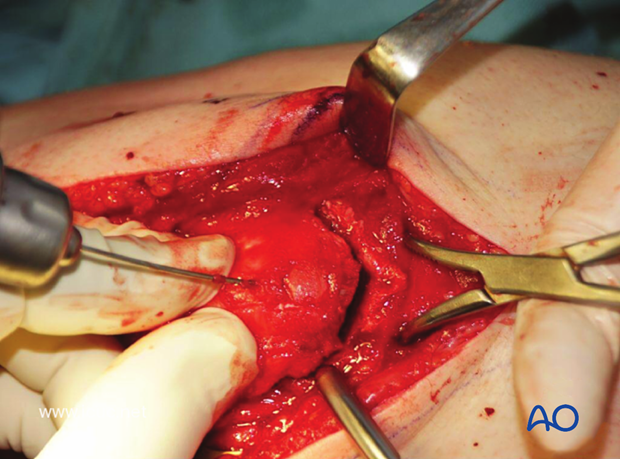
A hook plate is applied over the longitudinal K-wires to complete the fixation of the osteotomy.
The osteotomy is nicely reduced with the hook plate.
Lateral X-ray demonstrating the hook plate reduction of the Chevron osteotomy.
Final closure

Final X-ray images