ORIF
1. General considerations
Fracture-dislocations of the carpometacarpal (CMC) joint may involve articular fractures of the metacarpal base which require, after reduction of the dislocation, a separate reduction and fixation.
The metacarpal base fractures are fixed according to their fracture pattern.
If there is persistent joint instability, the joint may be stabilized with a temporary K-wire. In noncompliant patients, K-wire stabilization is recommended.
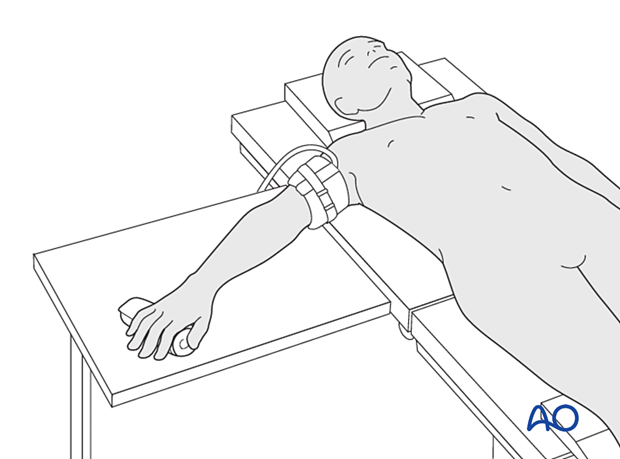
2. Patient preparation
Place the patient supine with the arm on a radiolucent hand table.
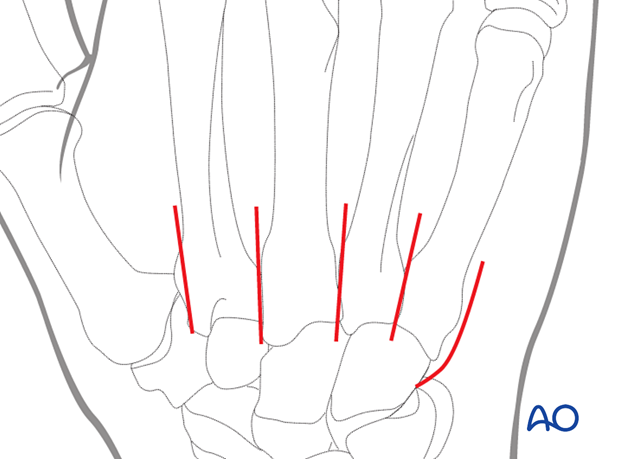
3. Approaches
A dorsal approach to the affected CMC joints may be used.
Alternatively, the approach(es) for reduction and fixation of the metacarpal base fracture can be used.
Protect the dorsal sensory nerve branches (radial and ulnar).
4. Reduction of dislocation
Dislocation is usually dorsally and may be reduced manually in a closed manner.
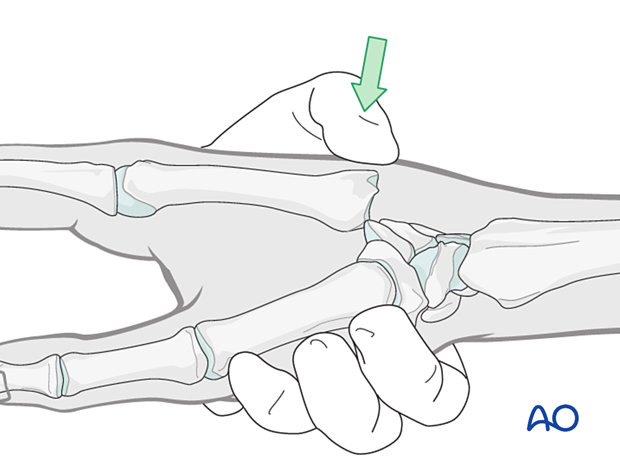
Interposed soft tissues or bony fragments, as well as irreducible fractures may require exposure of the joint to achieve satisfactory reduction. Often, the joint capsules are ruptured, and the joint space is easily exposed.
5. Reduction and fixation of fractures
Reduce and fix the fractures similar to isolated fractures.
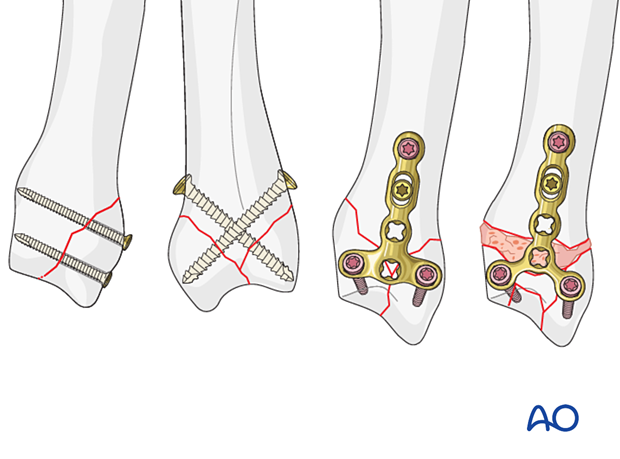
Partial articular fractures:
Complete articular fractures:
6. Stability evaluation
Confirm reduction and fixation with an image intensifier and check the joint stability by active flexion and extension. This should show congruent movement compared with the adjacent joints.
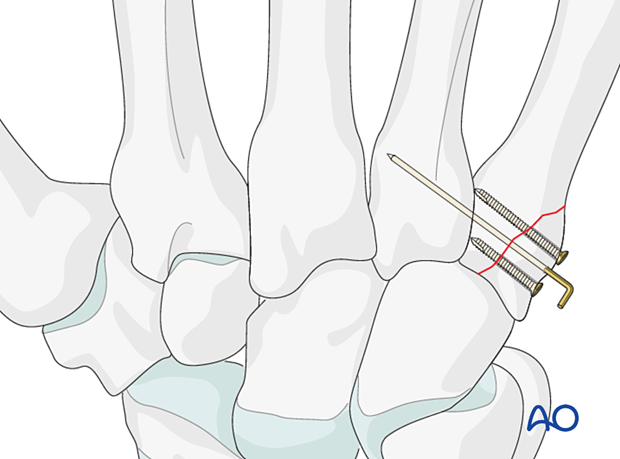
7. Joint stabilization with a temporary K-wire
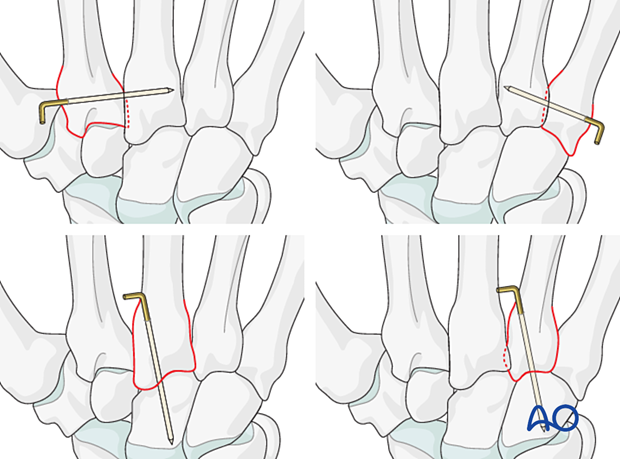
Often there is persistent instability, eg, subluxation or redislocation during the range of motion. In this case, add a temporary K-wire:
- Transverse fixation of the affected metacarpal base to an uncompromised neighboring metacarpal base
- Retrograde transfixation through the metacarpal base into the carpal bones
Repair the capsule.
Bend the end of the K-wire above the skin and cut it with enough length to avoid migration.
8. Aftercare
Postoperative phases
The aftercare can be divided into four phases of healing:
- Inflammatory phase (week 1–3)
- Early repair phase (week 4–6)
- Late repair and early tissue remodeling phase (week 7–12)
- Remodeling and reintegration phase (week 13 onwards)
Full details on each phase can be found here.
Postoperative treatment
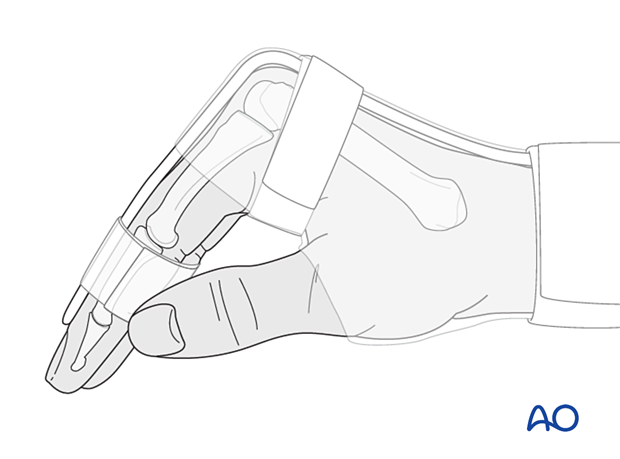
Support the hand with a dorsal splint for about 2–4 weeks. This would allow for finger movement and help with pain and edema control. The arm should be actively elevated to help reduce the swelling.
Pain control
To facilitate rehabilitation, it is important to control the postoperative pain adequately.
- Management of swelling
- Appropriate splintage
- Appropriate oral analgesia
- Careful consideration of peripheral nerve blockade
Follow-up
X-ray checks of joint position have to be performed immediately after the splint has been applied.
Follow-up x-rays with the splint should be taken after 1 week and possibly every 2 weeks.
The K-wire can be removed 4–6 weeks after surgery.
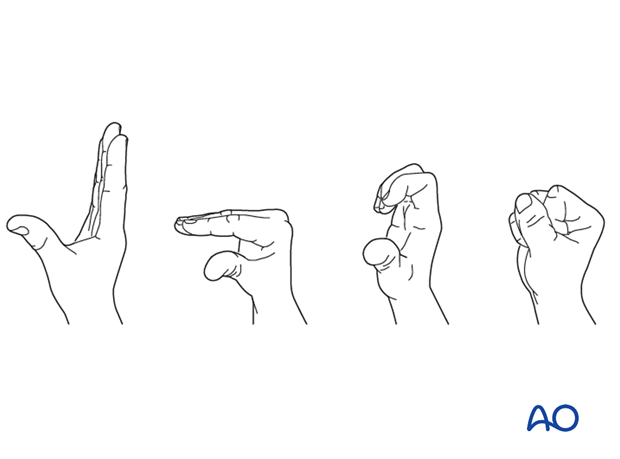
Splint immobilization is continued until about 4 weeks after the injury. At that time, an x-ray without the splint is taken to confirm healing, and range of motion should be pain-free.
Mobilization
Splinting can then usually be discontinued, and active mobilization is initiated. Functional exercises are recommended.
Implant removal
The implants may need to be removed in cases of soft-tissue irritation.
In case of joint stiffness or tendon adhesion restricting finger movement, arthrolysis or tenolysis may become necessary. In these circumstances, the implants can be removed at the same time.












