Complications
1. Complications of the injury
Complications may comprise:
- Nerve injuries
- Blood vessel injuries
- Open fractures, ie, breached skin
- Polytrauma patient
Clinical examination and documentation are necessary, particularly before any intervention. Further investigation using angiography or ultrasonography can be helpful for planning in the event of suspected neurovascular injury, but if there is any doubt about the integrity of a nerve at risk or distal limb perfusion, operative intervention is indicated.
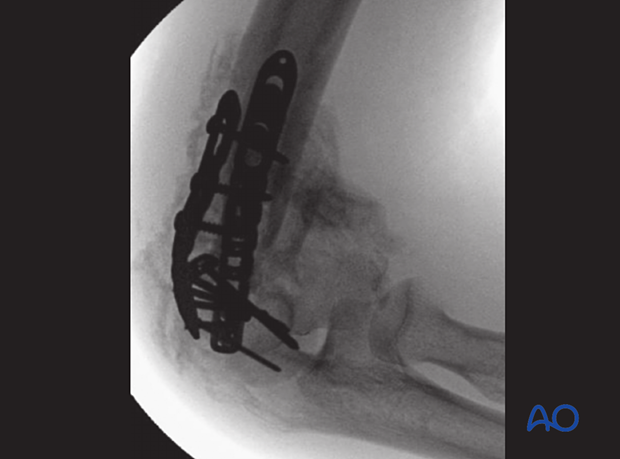
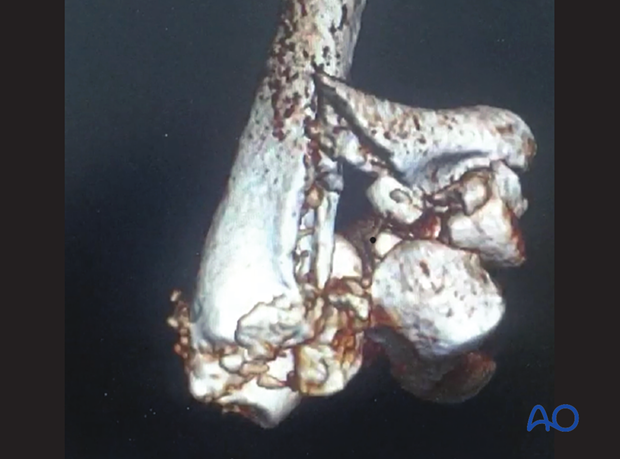
The case shown here is an open multifragmentary fracture Gustilo-Anderson type IIIa.

2. Complications of the treatment
Immediate complications
Immediate complications comprise intraoperative damage to:
- Nerves
- Blood vessels
Respect the neurovascular anatomy of the elbow (see the additional material on vascularization of distal humerus and neurological anatomy, protection, and handling).
It may be difficult to recognize that damage has occurred to nerves and blood vessels, but the clinical suspicion of damage should remain high, and the threshold to appropriate intervention should remain low. If there is any doubt, perform appropriate on-table angiography or exploration of the nerve or blood vessel.
Early complications
Early complications comprise:
- Neurologic injury (neuritis, paresthesia, or motor deficit)
- Compartment syndrome
- Infection
- Loss of reduction and/or dislocation
In the first three weeks of injury or intervention, swelling is common. Prevention of swelling helps to avoid delayed neuropathy and poor perfusion. It may also help to reduce the subsequent stiffness and heterotopic ossification.
The treatment of swelling includes:
- Release of circumferential bandaging acting as a tourniquet
- Elevation of the limb
- Early mobilization of the hand and forearm
Early neurologic deficit is usually due to swelling, traction injury, or irritation from hardware. It is essential that at the end of the procedure, the relevant nerves are visualized and their status documented. If this has been done, an expectant policy is recommended for most neurologic injuries. Each case should be considered individually.
Late complications
Late complications comprise:
- Delayed nerve palsy (due to malunion or malorientation, potentially nonreversible)
- Persistent or recurrent instability
- Stiffness and heterotopic ossification
- Arthritis
Stiffness may be caused by articular malreduction or capsular contracture with or without heterotopic ossification. Persistent instability and articular malreduction will result in arthritis. Instability and stiffness may coexist. Stiffness may also be neurogenic in origin.
Prevention and treatment:
- Prevention of instability and stiffness relies on accurate operative treatment and early rehabilitation.
- Treatment of instability in the presence of arthritis may be difficult and result in arthroplasty.
- Treatment of instability in the absence of arthritis relies on the assessment of the direction and magnitude of displacements during stress testing.
- Late ligament reconstruction can afford reliable outcomes.
Treatment of stiffness depends on the etiology: capsular releases and removal of heterotopic ossification may be helpful in restoring movement, but pain may still be a problem.