Infection
1. General introduction
Introduction
A fracture wound, whether traumatic or surgical, that becomes infected almost always results in prolonged treatment and a suboptimal outcome.
Any surgeon who treats fractures should be aware of risk factors for infection. Every effort should be made to reduce the risk of infection by following the basic surgical principles of fracture care.
Débridement: definition
The factors that reduce a patient’s ability to resist infection should be corrected whenever possible.

All necrotic, and infected, tissue should be removed surgically. The surgical removal of infected tissue is the mainstay of management of infected fractures. Such surgery is frequently referred to as débridement. Unfortunately this term, although an official Current Procedural Terminology (CPT) code of the American Medical Association, is open to interpretation and denotes different procedures in different surgical contexts and is not clearly defined.

Débridement, as used in this discussion, means the surgical exposure of the whole pathological zone and the removal of all necrotic, contaminated, damaged and/or infected tissue, whether bony or soft-tissue. All loosened hardware should be removed as well.

Principles
Infected wounds should never be closed until all infection is overcome and their condition permits.
Fractures should be stabilized surgically. Internal fixation devices can compromise local host resistance, and need to be removed unless they provide absolute stability, and the infection responds promptly to treatment. If an internal fixation device has to be removed prior to bone healing, then fracture stabilization by external fixation becomes necessary.
Bacteriology
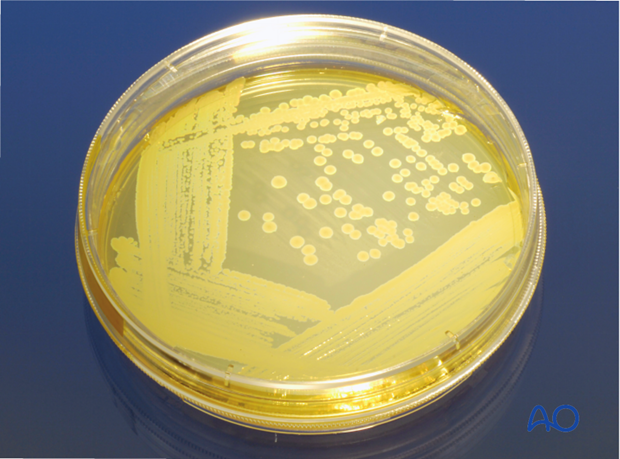
Infecting microorganisms should be identified, their antibiotic sensitivities defined, and appropriate specific antibiotics administered as an adjunct to surgical treatment.
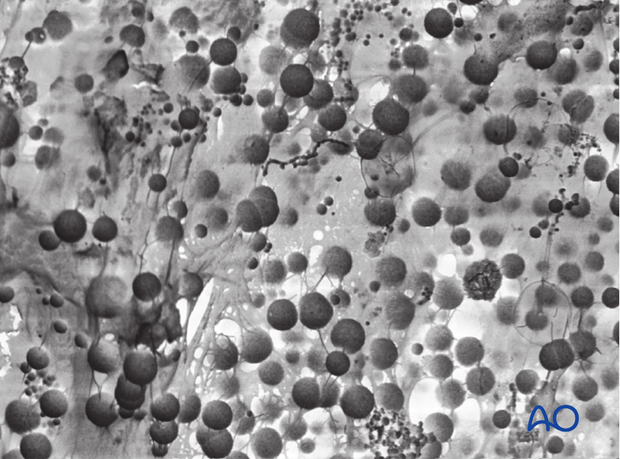
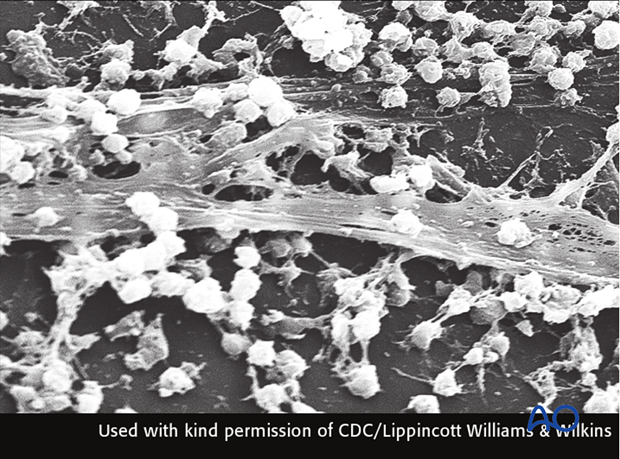
It is now appreciated that not all infecting micro-organisms are free in the wound tissues and fluids. Those that are free, and therefore likely to be detectable by standard culture techniques, are called, in modern terminology, planktonic micro-organisms.

Many of the bacteria that inhabit chronic wounds set up complex polymicrobial biofilm communities that can only be detected by culture techniques when they happen to detach a sufficient bolus of planktonic cells that can be grown on conventional culture media.
A major problem in bony infections is the fact that biofilm bacteria cannot be recovered by standard culture techniques, which means that fracture repairs often yield negative culture results even when multiple clinical signs point to infection. New techniques such as sonication can increase the yield of the cultures. It is important to realize culture results are affected if the patient is being treated with antibiotics at the time of culture.
2. Diagnosis of wound infection
Introduction
Early identification of a wound infection is the first step towards the prompt intensive treatment necessary for optimal results. Any wound communicating with a fracture, whether due to the injury, or created by a surgeon, is at risk of becoming infected.
Recognition of those factors that predispose to infection should increase the surgeon’s alertness to the possibility of infection. Early signs of infection are not specific and may easily be misinterpreted, as an inflammatory response is normally present in the region of a fracture, even without infection. Often, the first sign of wound infection is that the inflammation fails to resolve as quickly as expected. Certainly, increasing signs of inflammation (wound drainage, redness, swelling, pain and tenderness, fever) must be regarded as indicators of likely infection.
If the surgeon is concerned about infection, all steps to diagnose, or exclude, this possibility must be taken, as a matter of urgency.

Evaluation of possible infection
The presence of bacteria in an inflammatory wound exudate is proof of infection. Often this is most readily obtained by sterile aspiration of the wound, or preferably by surgical exploration. Microscopic examination (Gram’s stain) of the exudate, and appropriate microbiological cultures may provide evidence of bacterial presence. It has to be borne in mind, however, that there may be few planktonic bacteria in the wound and that most bacteria may be trapped in biofilms (see General introduction).
Prior antibiotic treatment may interfere with microbiological studies. Occasionally, increasing inflammation is evident without recoverable bacteria, but infection must be assumed if the clinical indicators are strong.
Systemic signs of inflammation, often associated with infection, are provided by several laboratory studies (see below). By themselves, none of these proves, or excludes, infection. The diagnosis of such infections is dynamic and based on serial clinical and laboratory observations. It is the duty of any fracture surgeon to monitor each patient closely for this serious complication.
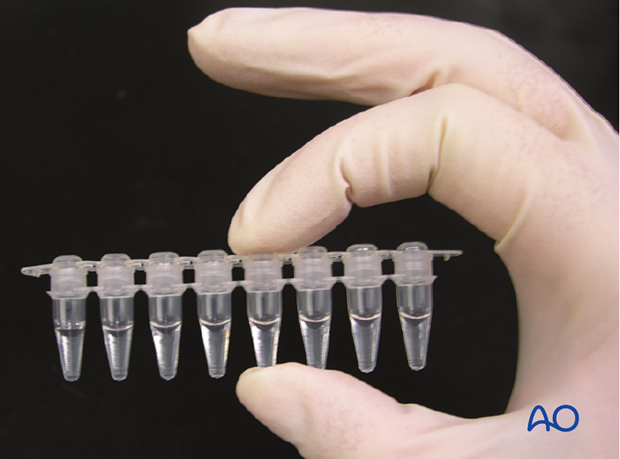
Note: PCR
Rapid advances in the use of molecular detection techniques have recently become available to clinical laboratories, using real-time polymerase chain reactions (PCR) and appropriately selected microarrays. This technology can rapidly identify selected bacteria, based on their DNA, as well as any antibiotic resistance. Microbiological culture is not necessary to use these techniques. As examples, it is possible to discover methicillin-resistance of S. aureus within a few hours, as well as to identify fastidious microbes, and those suppressed by antibiotics. Working with microbiologists using PCR, surgeons may well improve adjunctive antibiotic treatment, as well as improve diagnosis and classification of skeletal infections.
Relevant observations include:
- Serial wound examinations under aseptic conditions
- Maximal daily temperature reading
- Full blood count (FBC) with differential white cell count
- Erythrocyte sedimentation rate (ESR)
- C-reactive protein (CRP)
- Bacteriology (gram’s stain, culture and sensitivity)
- Imaging - Plain x-rays, (PET), CT scan, MRI, Indium111-labelled white blood cell scan, Technetium 99m labeled phosphate bone scan.
Classification of infection
An important guide to treatment is provided by the discipline of classifying an infection according to several parameters:
- duration of infection
- anatomical location
- host resistance to infection
- infecting organism(s)
- status of fixation
- status of bone healing
- viability of bone and soft tissues
Optimal management of an infected fracture or infected nonunion requires assessment of each of these factors.
Clinical examination
Serial observations of clinical symptoms and signs are most important for identifying the presence of infection. Increasing pain, seepage (either purulent or serosanguinous), swelling, redness, warmth and tenderness all suggest the possibility of a wound infection. Progressive worsening of one, or more, of these parameters is confirmatory. While some inflammation is caused by a fracture and by any operation to treat it, its severity should normally progressively decrease.

Imaging
X-rays
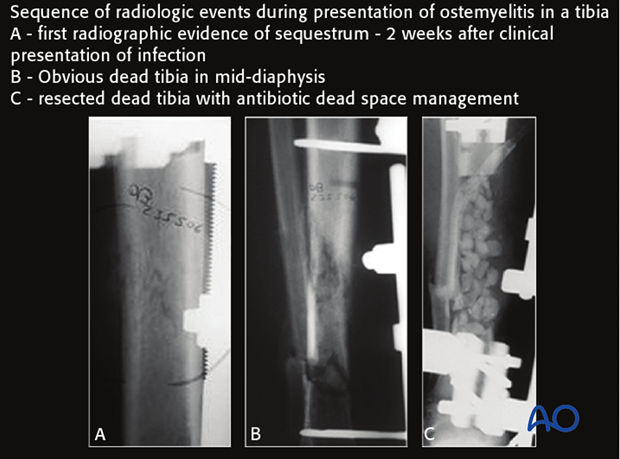
In the diagnosis of early infections, x-ray imaging plays a negligible role. Radiographic findings of infection are usually not evident until at least 2 weeks after the onset of infection, even though bone involvement has already occurred.
Imaging becomes important in the later stages of infection. It is helpful to examine serial x-rays for progressive changes that could suggest infection.
Radiographic signs are neither sensitive nor specific for infection; e.g., radiographic evidence of implant loosening may be present as a result of instability, infection, or both.
Ultrasound
Ultrasound is useful to identify any accumulation of fluid (hidden abscess). The method is non-invasive and may image deeper layers, especially in the thigh. Ultrasound can be helpful for guiding diagnostic needle aspiration.
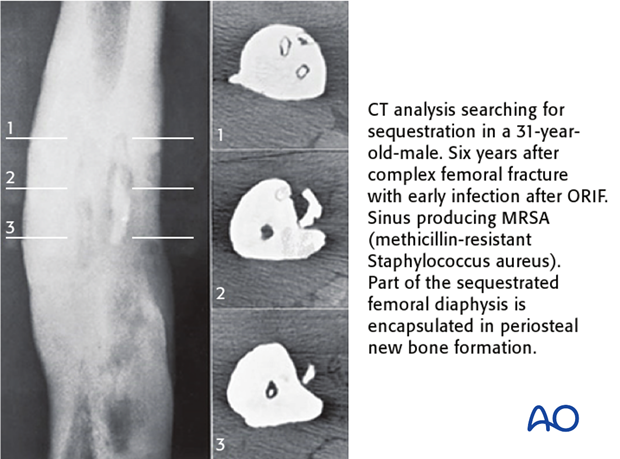
CT
Computed tomography offers a cross-sectional guide for exploration and excision, particularly of bone fragments (sequestrum).
As with plain radiographs, CT scans offer no specific diagnostic signs for, or against, infection, and is rarely useful in early infections.
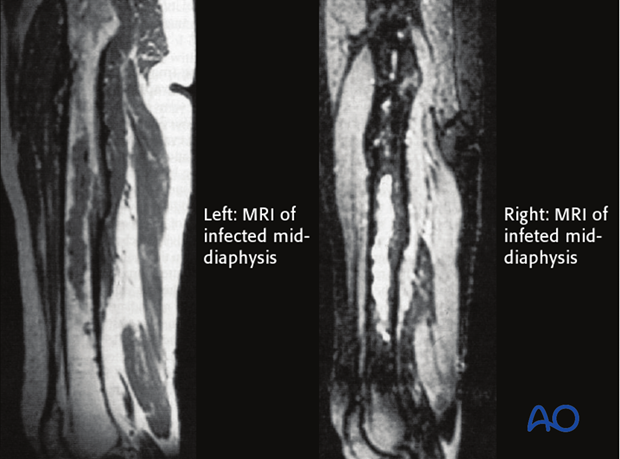
MRI
MRI offers improved imaging of soft-tissue abnormalities and can show greater anatomical detail than other imaging methods. Again, MRI signs of infection are non-specific. A disadvantage of MRI is the problem of artifact related to ferrous metallic implants. Titanium implants produce less interference.
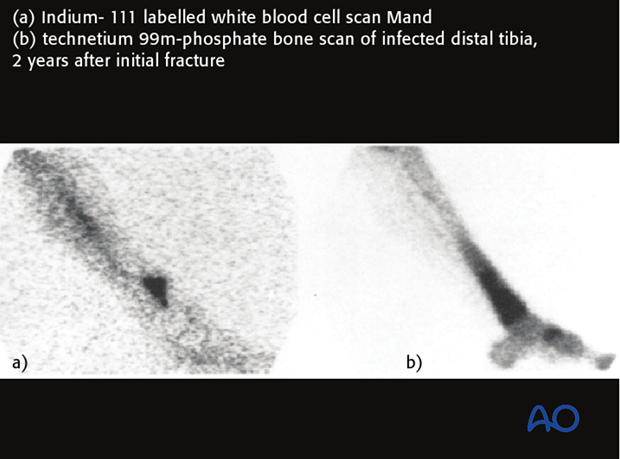
Bone scan
Uptake of technetium 99m-labelled phosphate compounds (TCN-MDP) by bone is increased in areas of higher vascularity, including infections and bone healing. With infection, a 3-phase bone scan shows increased uptake of labelling in all 3 scan phases.
Absence of uptake suggests impaired vascularity, or bone necrosis. Bone scanning detects increased bone remodeling that is present around all fractures for 12-24 months. Bone scanning cannot differentiate aseptic hardware loosening from infection. Bone scans are of negligible value in the early postoperative period of acute fractures.
Indium111-labelled white blood cell scans are more specific for inflammation and infection. The illustration shows a larger area of uptake, surrounding hyperemia and inflammation with TCN-MDP (b) than with the indium111 white blood cell technique (a). However, false positives and false negatives still occur, and such scans can be positive in un-united fractures.
Bacteriology
If an infected area is to be explored, preoperative aspirate of fluid accumulation and especially intraoperative tissue sampling from several potentially infected sites, prior to the start of any antibiotics, provide the best material for detecting the infecting microorganism(s). At least 5 specimens should be taken for microbiology testing. One sample should be sent for histopathology. Both aerobic and anaerobic cultures should be undertaken. PCR, if available will speed up, and make more reliable, the characterization of the organisms. If hardware is removed, this can be cultured as well preferably after sonication.
Histological investigation can reveal a bacterial etiology, even if the microbiological tests are negative. Superficial wound swabs should be avoided because of low sensitivity and frequent contamination by surface organisms. Ideally, prior to tissue sampling for culture, it is important to discontinue any antibiotic therapy for at least a week.
Septic arthritis
If the infection is suspected to involve a joint cavity, there is a need for drainage, surgical clearance and irrigation of that space. At the slightest suspicion of septic arthritis, joint aspiration should be performed to evaluate the affected joint. If infected fibrinous deposits (cloudy aspirate) are present with positive cultures, then arthroscopic or open irrigation should be performed repeatedly, every 2-3 days, until the infection resolves. If arthroscopic clearance is unsuccessful, one should proceed with open synovectomy.
If there is articular cartilage degradation, arthrodesis may become unavoidable.
3. Classification of fracture wound infection
Introduction
A variety of factors can influence the prognosis of fracture wound infections. Unlike hematogenous osteomyelitis, a fracture wound begins with damaged soft tissue and bone, and consequent, locally-reduced resistance to infection. There may also be necrotic bone, and perhaps foreign material, where bacteria are protected from host defenses and blood-borne antibiotics, often sheltering in biofilms (see General introduction).
Factors to consider in categorizing infections are:
- duration of infection
- anatomical area of bony involvement
- host resistance (systemic and/or local)
- status of fracture fixation
- status of fracture healing
- microbiology
Classification according to chronology of onset of infection
The time of onset of fracture-site infection is relevant, since progressive infection leads to additional tissue damage and spread of infection outwards from the original infected locus. The diagnosis of infection within 2 weeks of injury or the first open intervention is to be regarded as an early infection. Diagnosis after two weeks may suggest that the infection was dormant for a period before declaring itself. The diagnosis of late infection generally implicates more extensive tissue pathology than if picked up earlier.
Early presentation of infection
Infection, diagnosed in the first two weeks after injury or after the first surgical intervention, is likely to have caused less tissue damage, than if discovered later.
The treatment of all fracture wound infections is urgent and is primarily surgical, with antibiotics as an adjunct.
There is no place for the administration of antibiotics and a “wait and see” approach.
Click here to read more about early presentation of infection.

Later presentation of infection
Infection may not be seen until several weeks after surgery.
More extensive and intensive treatment is usually necessary.
Click here to read more about delayed presentation of infection.

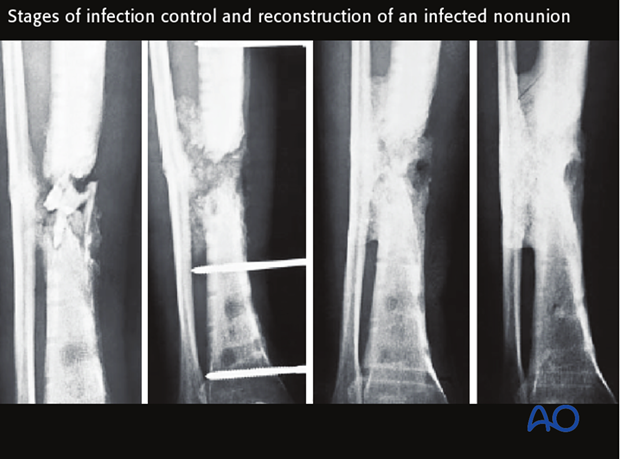
Chronic fracture wound infection
Late presentation, chronic infection is associated with extensive infection of tissues and dead bone, sometimes sequestered.
Treatment relies on
- total surgical removal of all dead and infected tissue, including bone
- removal of implants
- placement of an antibiotic spacer
- re-stabilization of the fracture, using external fixation
- appropriate adjunctive antibiotic therapy
Click here to read more about chronic fracture site infection.
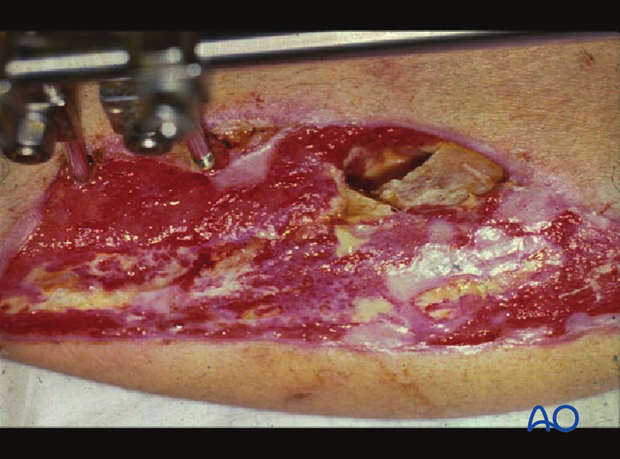
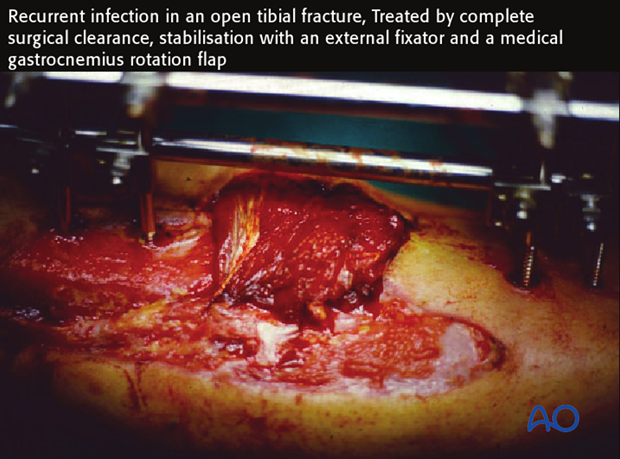
Recurrent osteomyelitis
Posttraumatic osteomyelitis may recur, sometimes years after the original infection appeared to have resolved.
Treatment depends on:
- fracture healing
- implants
- sequestra
Treatment relies on:
- Surgical removal of all infected and dead tissue
- Identification of the responsible microorganism from cultures of biopsies
- Fracture stabilization, as necessary, with external fixation
- The use of appropriate adjunctive antibiotics
- Soft-tissue reconstruction, once infection is eradicated
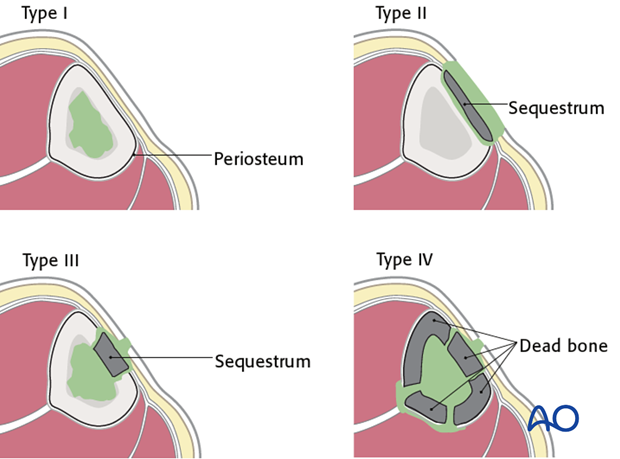
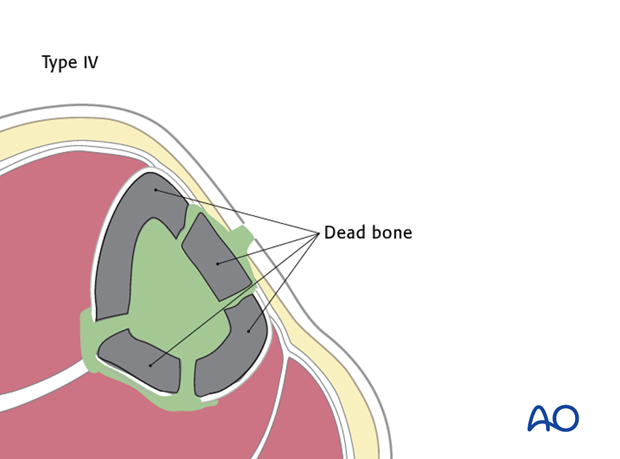
Cierny’s classifications
Cierny has classified fracture site infections according to a number of criteria:
- anatomical
- host resistance
- microbiology and
- the status of fracture healing.
These are all important factors to be taken into consideration.
4. Treatment - initial surgery for fracture wound infection
Introduction
If an infection is strongly suspected, the surgeon must proceed urgently to exploration of the wound, obtaining tissue for culture, and removing all non-viable tissue and exudates.
Such débridement (see below) involves the surgical excision of all necrotic and/or infected tissue from the wound.
Débridement must include:
- Wide exposure of the whole pathological zone
- Removal of all exudate (hematoma and pus)
- Removal of the abscess membrane
- Removal of sinus tracts
- Removal of granulation tissue
- Removal of unhealthy wound margins
- Removal of all dead bone
- Removal of loosened hardware
Look carefully for dead bone and any remaining foreign material. Preserve nerves, identifiable blood vessels and viable tendons.

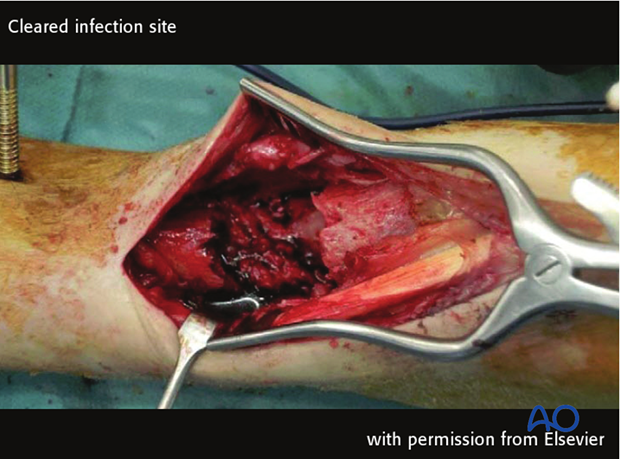
Débridement
The surgical excision must be complete and thorough.
Adequate, timely débridement is the most important element of the treatment of a fracture-wound infection.
With well-established infections, there may not be a clear demarcation between viable and non-viable tissue. Radical excision may be necessary to eliminate infection, even though it may increase the complexity of reconstruction.

After débridement, the surgical site should be thoroughly irrigated with normal saline solution to reduce the bacterial population. The use of pulsatile lavage has been questioned as the water jet might transport bacteria deeper into the soft tissue. In cases with large amounts of dead tissue, or grossly purulent wounds, repeated surgical clearances are indicated. Deciding what tissue to remove and what tissue to retain is the essential challenge of débridement. Such decision-making is learned from experienced surgeons and by practice. Common errors are failure to remove enough compromised tissue, and/or to do so in a way that injures the retained tissue. An organized approach that proceeds in orderly steps through tissue levels is required. Any non-viable skin is excised. The incision should be extended, as necessary, for adequate exposure of the whole infected zone. The depths of the wound are then exposed, and must include all of the previous surgical exposure. Any extension of hematoma, pus, or necrotic tissue, should be explored fully.

With acute wound infections, internal fixation devices may be retained, if they continue to provide absolute mechanical stability. If the implants are loose, and in more established infections, it is advisable to remove all hardware and to re-stabilize with an external fixator. Make sure to position the pins far enough from the infected wounds, while still maintaining adequate stability.
Excise the surface of the exposed tissue to leave clearly viable margins of subcutaneous tissue, fascia and muscle. Non-viable bone must also be removed with a high-speed burr (suitably irrigated to cool the tissue), or preferably osteotomes, until bone bleeding is encountered. Small bleeding osseous vessels (“paprika sign”) indicate viable bone.
Copious irrigation with Ringer-lactate solution helps to remove bacteria, bits of dead tissue and blood clot, and improves the surgeon’s ability to examine the wound.
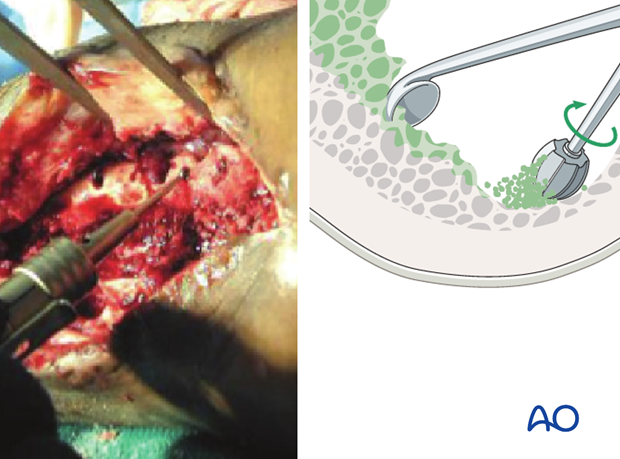
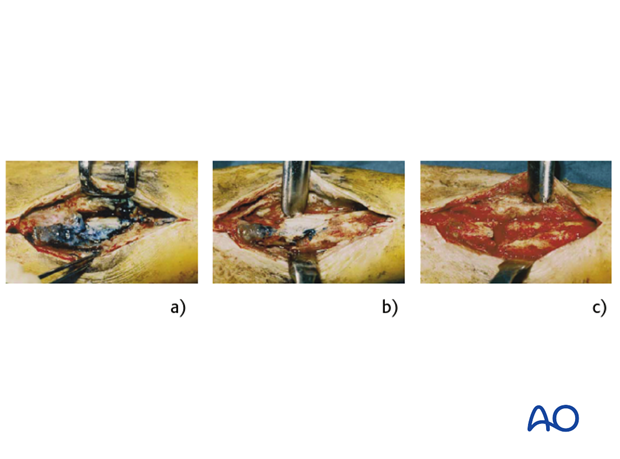
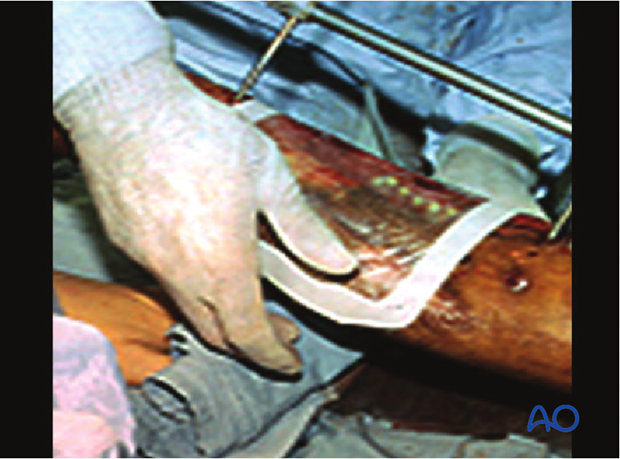
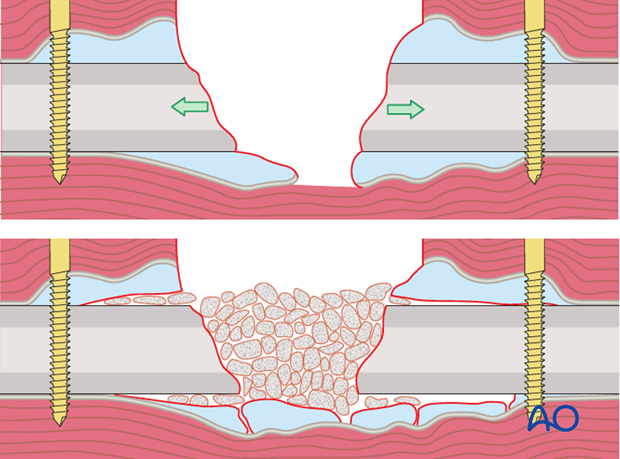
A “second look” and possibly further débridements should be undertaken, until the wound surface is completely viable. Staged surgical clearance is illustrated.
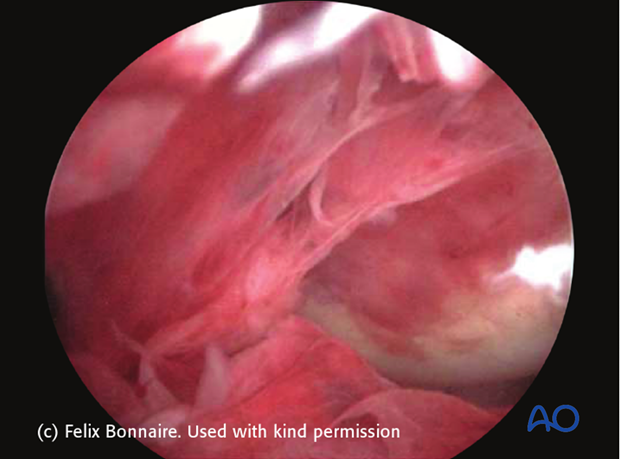
Local débridement of an infected nonunion is characterized by:
a) The nonunion is covered by granulation tissue, stained with methylene blue, previously injected into the sinus.
b) After excision of the granulation tissue, the necrotic bone adjacent to the nonunion contrasts directly with the vital bone.
c) After complete surgical clearance, only vital bleeding bone and soft tissue is seen.
5. Treatment - management of the fracture wound
Initial antibiotic treatment
Before starting therapeutic antibiotics, it is important to obtain adequate cultures, or PCR characterization (if available). At least 5 samples should be obtained in the operating room from different locations in the wound. Only if the patient has evidence of septicemia should antibiotics be given before wound exploration.
Selection of antibiotics for initial treatment is based on the antibiotic sensitivities of likely infecting organisms, including any results of previously positive cultures.
Generally, broad-spectrum, intravenous antibiotics are advisable as soon as cultures have been obtained. Initial antibiotics are selected, based on the results of gram’s stain, and on institutional frequency statistics (see table on left; Trampuz A, Zimmerli W (2006) Diagnosis and treatment of infections associated with fracture-fixation devices. Injury. 37 Suppl 2:S59-66.).
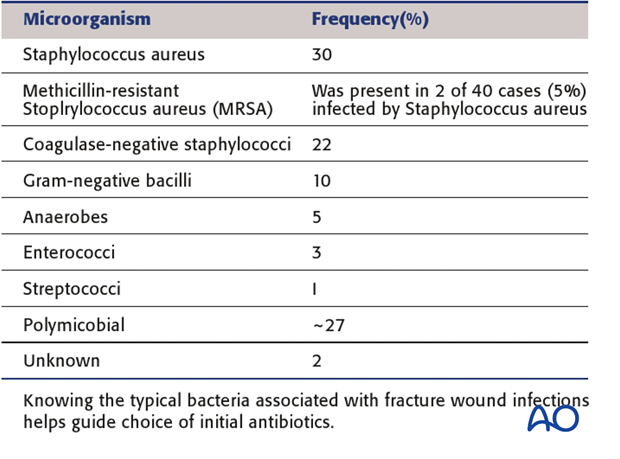
Methicillin-sensitive S. aureus (MSSA) is still the most likely infecting organism in most areas. Institutionalized patients have a higher risk of methicillin-resistant S. aureus (MRSA), in which cases vancomycin may be advisable.
Coverage with antibiotics active against gram-negative microorganisms is wise for hospital-acquired infections.
All of the above should be considered provisional treatment until culture results become available.
Definitive antibiotic treatment
Once culture results and sensitivities are known, choose the optimal antibiotic for the infection, in consultation with an infectious-disease specialist. Remember that antibiotics are but an adjunct to adequate surgical clearance, and recognize that an infection that does not respond will need repeat surgical exploration and clearance.
If laboratory services are limited, then the choice of antibiotics is determined by the most appropriate available for the most likely organisms.
Prolonged intravenous antibiotics (e.g., six weeks), the use of combinations of drugs, and continued oral medication after initial intravenous therapy may be necessary.
Dead space within the wound
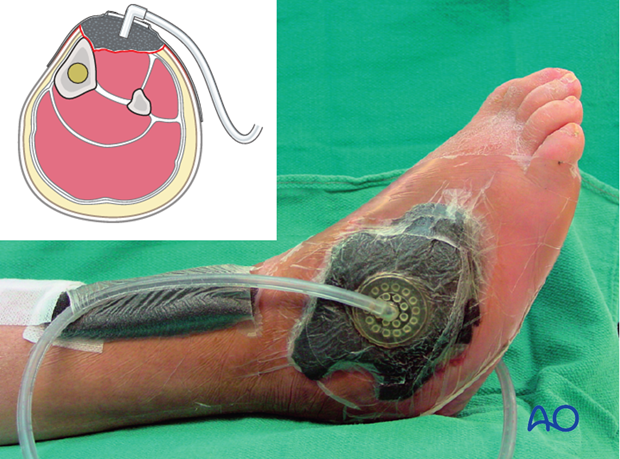
After the first surgical clearance of an infected fracture wound, it is essential to defer suture closure or other definitive soft-tissue cover. Closure may be considered when final clearance has resulted in resolution of the infection.
Empty space (“dead space”) under tissue flaps, or within bony cavities, within the excised wound allows further accumulation of exudate and is likely to become a reservoir of bacteria. Antibiotic levels will be low in this poorly-perfused accumulation of fluid.
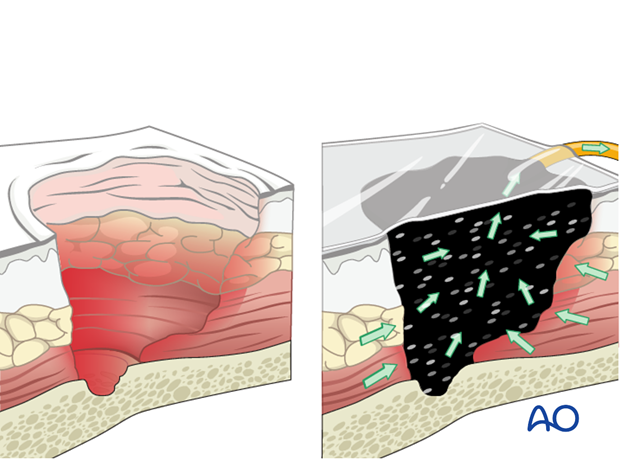
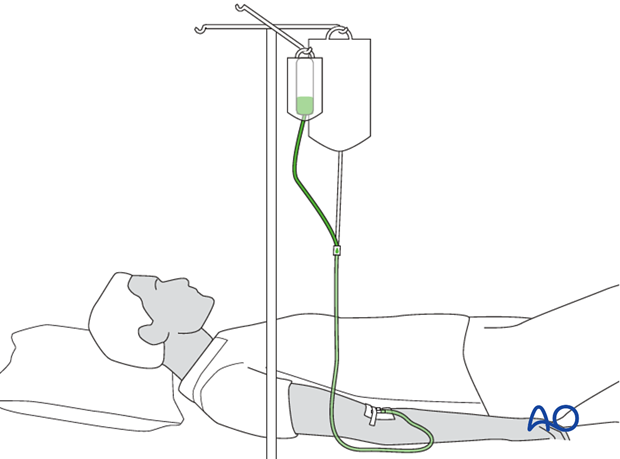
Filling this dead space is an important part of wound management. Alternative treatment strategies include the use of antibiotic beads, or other temporary space fillers (calcium sulphate, bone cement, etc.). The wound itself should be covered to avoid desiccation, or secondary contamination. This can be done with an impermeable dressing (adherent plastic), or with vacuum-assisted closure (VAC), as illustrated. The latter, by applying suction, reduces dead space volume in pliable tissues.
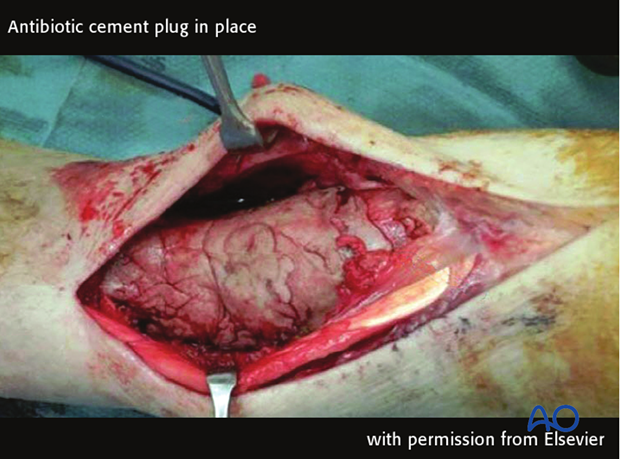
Dead space in bone
A significant bone defect may be filled with antibiotic beads, or other space fillers.
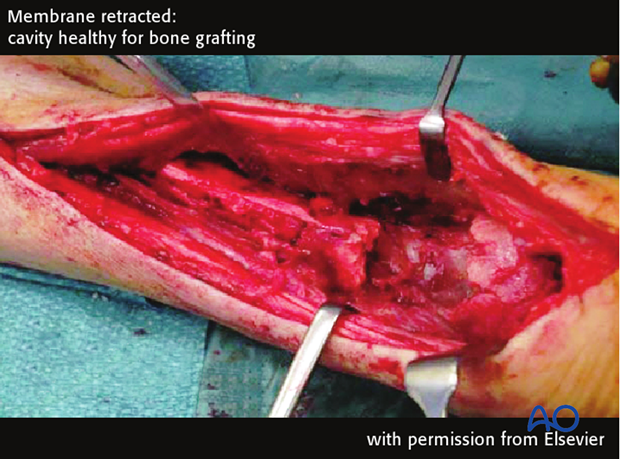
Recently, the technique of Masquelet has become popular. This involves the insertion into the bony defect of a solid antibiotic-containing cement spacer, which is left in place for 6-8 weeks while a membrane develops around it. The spacer is then removed and the surrounding membrane is filled with autologous bone graft. (The membrane has been studied extensively and it has been suggested that this membrane has osteogenic capacity.) This often consolidates when used for small to medium-size defects.
For more details see: Giannoudis PV, Faour O, Goff T, Kanakaris N, Dimitriou R (2011) Masquelet technique for the treatment of bone defects: tips-tricks and future directions. Injury 42(6):591-8. Case taken from article with permission from Elsevier.
Antibiotic cement plug in place. Make sure the cement fills the defect and also covers a few mmm of the cortex on either side of the plug. The cement can be prepared with addition of heat-stable antibiotics of choice.
Membrane incised 6 weeks later

Membrane retracted, cavity healthy for bone grafting
6. Treatment - implant retention or removal
Implant retention or removal: plates and screws
For as long as a plate and screws provide absolute stability, fracture healing can usually take place despite the presence of treated infection, notwithstanding the presence of a metallic foreign body. It appears that in most cases, stability is more important than the negative effects of the foreign body upon host defense.

Typically, fixation remains stable in early infections. However, at any stage, if the implants are loose, they must be removed. External fixation stabilizes the fracture while avoiding a metallic foreign body in the infected fracture wound, and is the best choice for early fracture destabilization in the presence of infection.

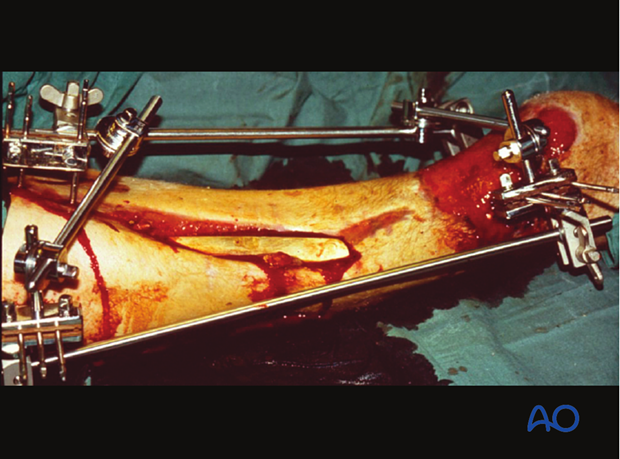
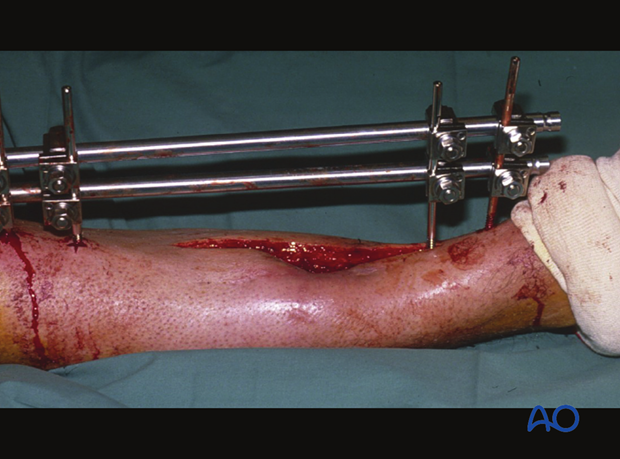
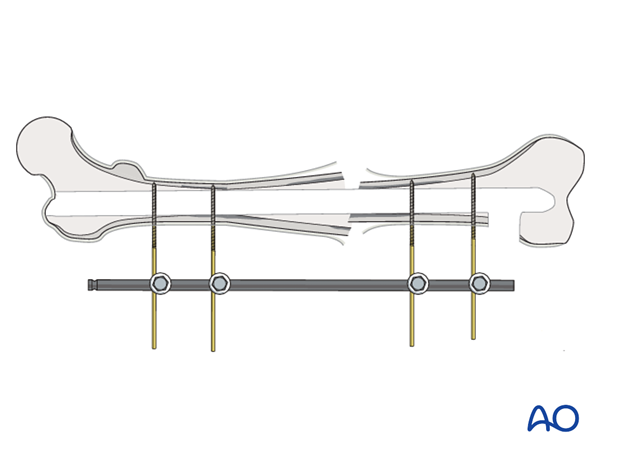
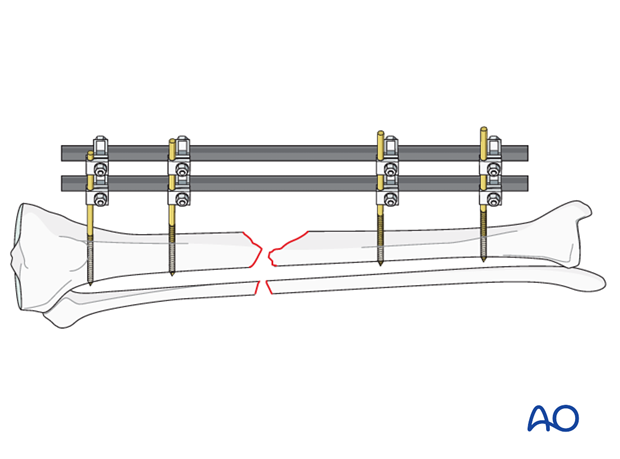
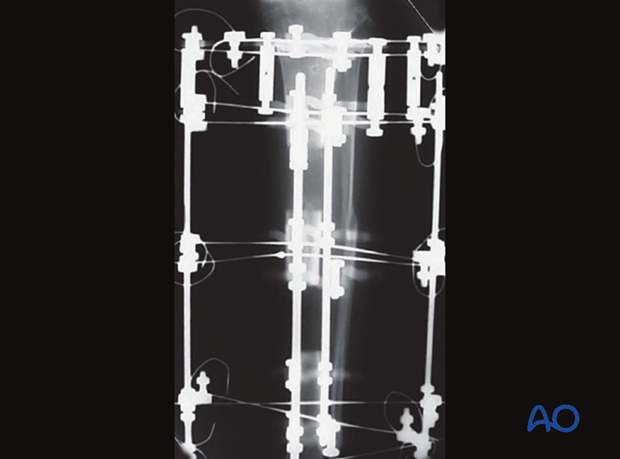
Stabilization with external fixation
The diagram demonstrates an ideal external fixation placement. The pins do not hamper surgical access to the infected zone, and are well-separated within each fragment, so as to provide optimal stability. Two bars also improve the strength of the fixation. The configuration should be planned carefully.
An external fixator can be used either as a temporary, or as a definitive, stabilizer. Even if definitive external fixation is planned, a temporary fixator may be best after initial débridement. This aids repeated clearance and wound care. Once further wound access is no longer required, a new fixator that provides optimal stability can be applied.
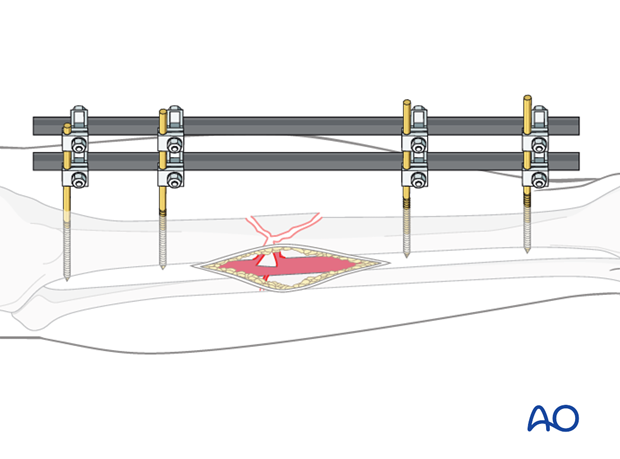
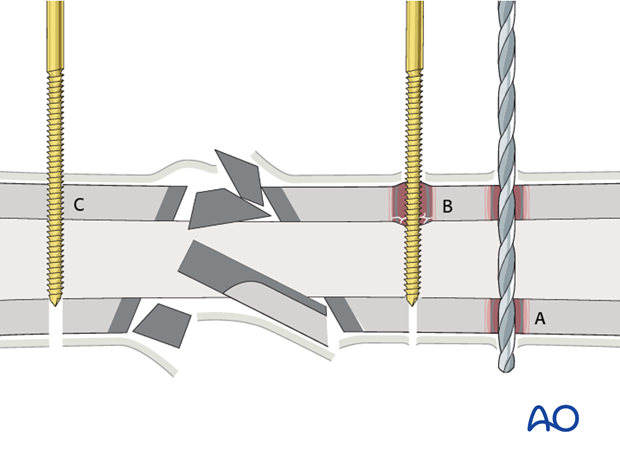
Mistakes in pin insertion for external fixation are:
- Drilling at excessive speeds or with a blunt drill bit (A), producing thermal necrosis of bone.
- Insertion of the Schanz screws, or pins, without adequate pre-drilling (B) causing microfractures, as well as excessive heat, which results in small necrotic bone fragments, or ring sequestra.
- Correct pre-drilling and correct pin/screw insertion (C) minimize the risk of pin tract infection.
Plates and screws
If an identified infection is treated early, and its fixation remains stable, then with appropriate surgical clearance and antibiotics, the infection is likely to respond and to remain suppressed during fracture healing. Despite successful fracture healing, later recurrent infection can lead to the need for hardware removal.
After the “infected hardware” is removed from the united fracture, and any necessary further excision of questionable tissue and/or bone has been undertaken, the infection usually resolves satisfactorily with a low risk of recurrence.
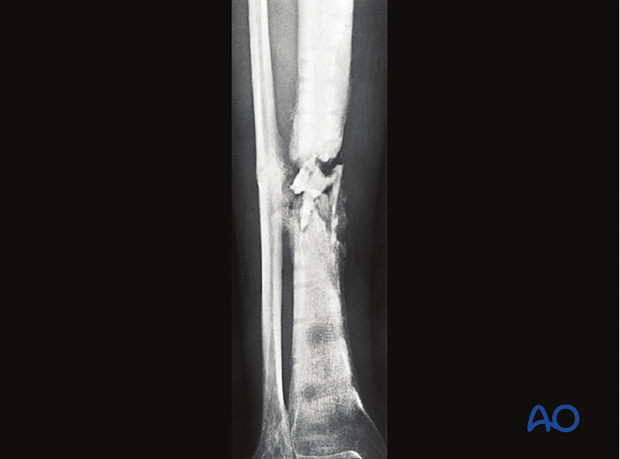
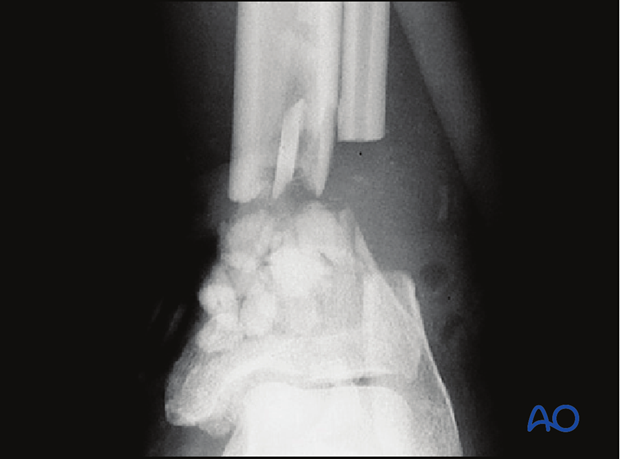
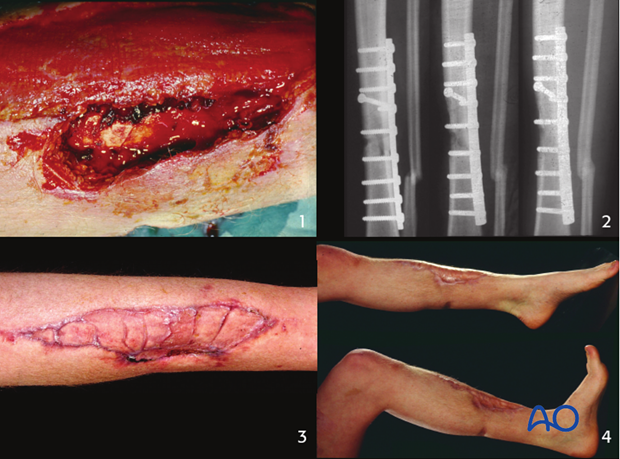
The pictures to the left: Plated tibia fracture. Early infection debrided. Plate was stable and left in situ. Eventual granulation over bone and then partial thickness skin grafting.
Implant retention or removal: IM nails
If a wound infection develops after intramedullary nailing, it is likely that the infection has spread along the medullary cavity. The infection may be early, or late, before or after union. Adequate surgical clearance requires removal of the nail and reaming of the medullary canal.
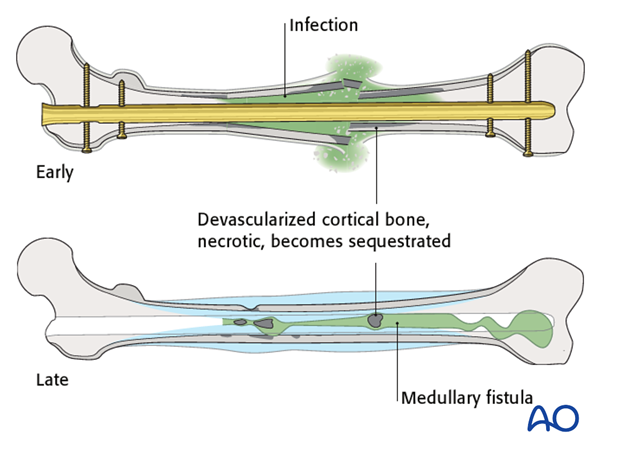
During initial clearance, a distal opening is created at the lower end of the nail tract, in order to allow debris from reaming to escape, and to drain the “sump”. The canal is then reamed to a diameter 1.5 mm larger than the removed nail, and is thoroughly and copiously washed out with Ringer-lactate solution. If there are obvious cortical sequestra, these need removal by open procedure.
An external fixator should be applied for stability, if the fracture is not healed.
If the infection is early and due to a less virulent bacterium, then renailing might be considered.
If the infection is late, or due to resistant organisms, external fixation is preferable to renailing.
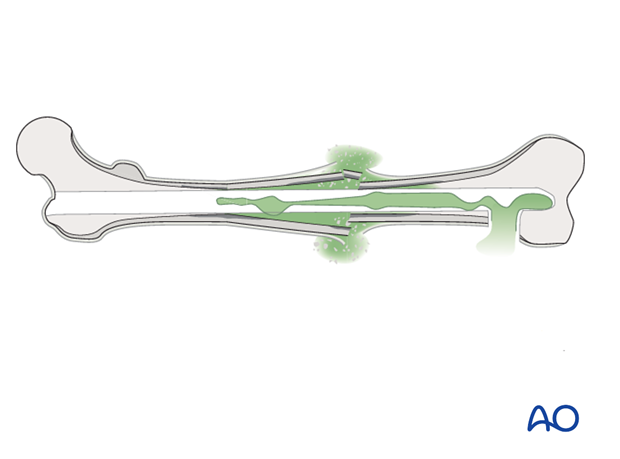
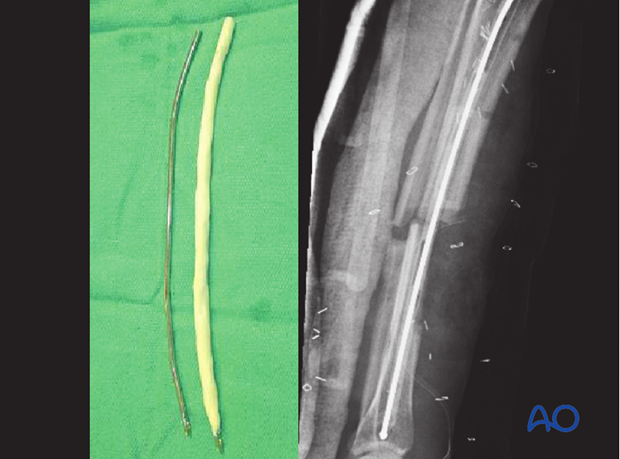
An alternative is to insert temporarily a reinforced, antibiotic-containing polymethylmethacrylate (PMMA) “nail” into the medullary canal, after reaming out the infective membrane and thorough lavage of the IM canal, also excising any sinus tract and any sequestra. An antibiotic-loaded PMMA nail is prepared by injecting liquid bone cement, pre-mixed with antibiotics (e.g. tobramycin 1 g per cement batch) into both ends of an appropriately sized chest tube which is vented in the middle to allow complete filling. A small-diameter flexible rod (e.g., nailing guide wire) is inserted before the cement hardens. The chest tube is then cut off.
The “nail” can be left in situ until the fracture has healed, or until the infection is under control, and then replaced with a solid metallic nail – a solid nail is used in order to avoid the hollow nail’s becoming a hiding place for bacteria.
Implant retention or removal: external fixators
Since external fixator pins are usually distant from the fracture wound, their removal is rarely required, but adjustment, or reinforcement, of the frame may be required to ensure alignment and stability.
Should an external fixator pin tract become infected, the pin should be removed, the pin site surgically cleared, and a new fixation pin placed into healthy bone. The pin tract clearance is best achieved with a drill and a bit slightly larger than the residual pin hole, together with copious irrigation. If it is anticipated that external fixator will be in place for longer (2-3 months) one can consider the use of hydroxy apatite coated pins. They have been shown to be less prone to loosen.
7. Treatment - wound closure and definitive stabilization
Wound closure
Following infection after ORIF (A, B) and after débridement has been satisfactorily completed, in one or more procedures (C), consideration must be given to choosing the best means of wound closure. Suture closure, particularly with skin tension, carries very high risks of wound healing problems. If possible, delayed primary suture closure can be considered. If this is chosen, however, the surgeon must watch carefully for wound breakdown, or recurrent infection.
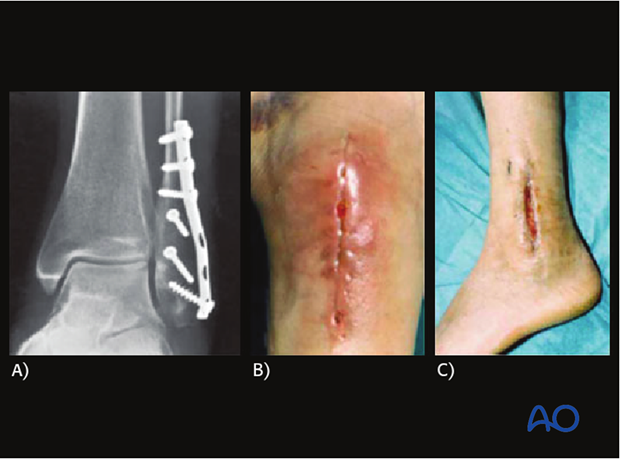
A safer alternative is to leave the wound open and allow it to heal by second intention (D), or with the use of split-thickness skin grafts. This is appropriate for wounds without exposed hardware, bone, cartilage, or other sensitive tissues.

If the wound is widely open, or tissue protection is necessary, some form of flap coverage will probably be necessary. A VAC can be used to reduce the size of an open wound and to promote granulation tissue. A clean granulating wound with a healthy viable base may be covered with a split-thickness skin graft. An alternative temporary dressing for an open wound is an impermeable adhesive drape to create a space (bead pouch) for antibiotic beads.
Closure with local, or free, flaps is often appropriate for larger and more complicated wounds, once the infection has been adequately cleared surgically.
It is important to close a complex wound as soon as is safe, rather than leave it open too long and risk secondary infection. The timing of these stages requires mature surgical judgment.
Fill dead space
Antibiotic beads
Surgical débridement of unhealthy soft tissue and/or bone may leave dead space between bone ends, or under flaps.
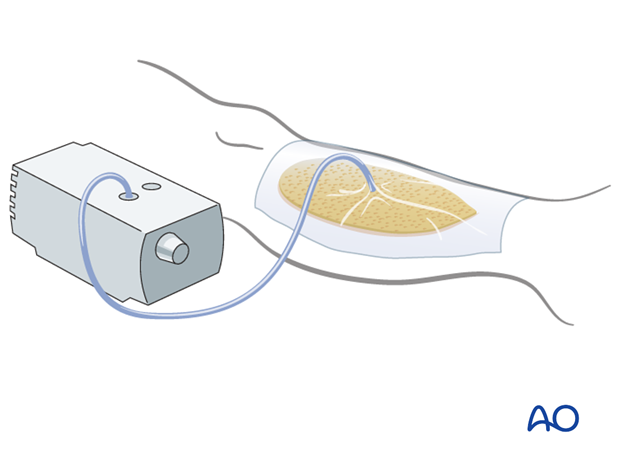
When the excised infected wound presents “dead space”, antibiotic-laden cement is frequently used, both to fill the space and to deliver locally high doses of antibiotic. A common technique is the use of antibiotic-laden polymethylmethacrylate (PMMA) beads.
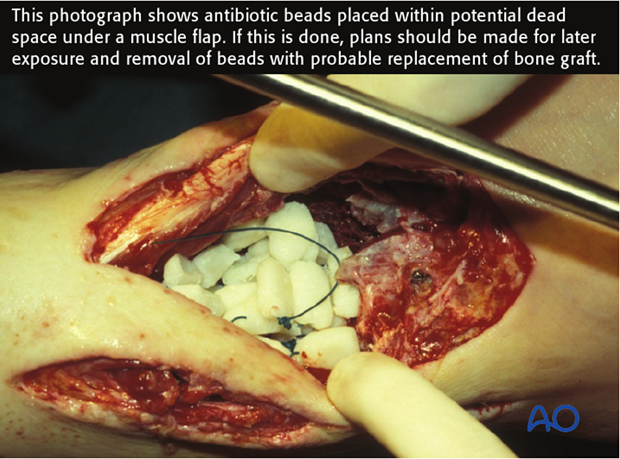
Antibiotic-impregnated beads may be purchased in some countries (at some expense), or made by the surgeon more cheaply. One gram of cefazolin (a first generation cephalosporin), or 1.2 g. of Tobramycin is mixed with each standard package of PMMA and, as it hardens, beads of 5 mm are carefully wrapped around a non-absorbable heavy nylon stitch (see adjacent photograph), knotted at intervals to prevent sliding of the “beads”.

Definitive stabilization
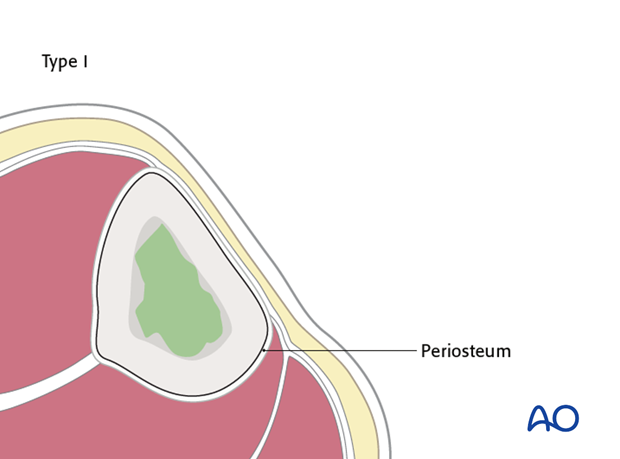
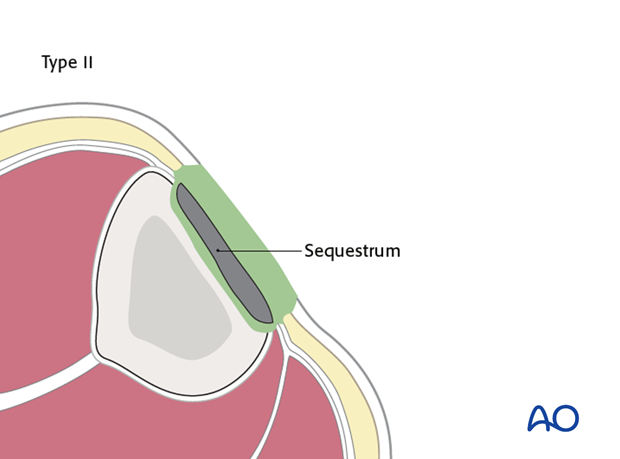
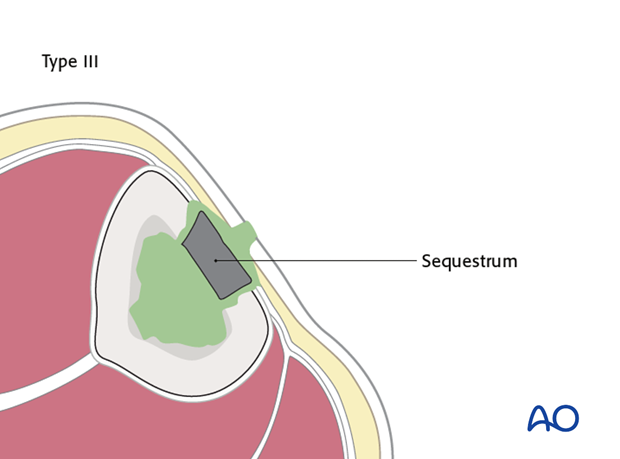
The anatomical classification ( see Cierny classification) of adult bone infection helps to determine the method of definitive stabilization when the fracture has not united.
Medullary osteomyelitis (type I) is usually associated with an intramedullary nail, which may, or may not, have been removed during initial surgery for infection. Once the tissue is healthy, the bacteria are sensitive, and the patient is systemically healthy, it may be appropriate to restabilize the fracture with another nail.
Superficial osteomyelitis (type II) is typical of a healed fracture with superficial bone necrosis, often deep to a plate. After removal of the plate, this superficial necrotic bone is removed with a burr, or a chisel, until underlying bleeding bone is reached. Replacement fixation is only needed if fracture healing is tenuous.
Wound coverage (closure, or partial thickness skin grafting) may follow soon after such superficial surgical excision, once resolution of the infection is assured.
Localized, full-thickness osteomyelitis (type III) may be associated with a ununited fracture. Surgical excision back to bleeding bone may remove so much cortex that the structural integrity of the bone is compromised and pathological fracture is a risk. Mechanical protection will then be necessary, using an external fixator. More complex options for soft-tissue closure (local or free flaps) may be required.
Bone grafting is often necessary, but should be delayed until soft-tissue coverage is healed and stable, and the infection has healed.
Diffuse osteomyelitis (type IV) causes widespread areas of infected and/or necrotic bone, so that extensive surgical clearance is necessary. This may result in a segmental defect. Such defects will require bone grafting, bone transport, or fixing in a shortened position if loss of length is acceptable.
Wounds associated with type IV posttraumatic osteomyelitis often need complex soft-tissue flaps for closure. Such widespread infection may justify amputation, especially in under-resourced healthcare environments.
8. Treatment - bone and soft-tissue reconstruction
Principles
After eradication of infection by surgery, combined with appropriate antibiotics, and the creation of a viable and stable soft-tissue environment, skeletal reconstruction comes next.
During the program to eradicate the infection, bear in mind the likely reconstructive options (bone graft, bone transport, or amputation), planning carefully incision placement and external fixator pin locations, etc., provided this does not compromise infection control.
Stabilization
Skeletal stability facilitates
- fracture healing
- enhanced wound care
- final reconstructive surgery (soft tissue and bony)
- functional aftercare
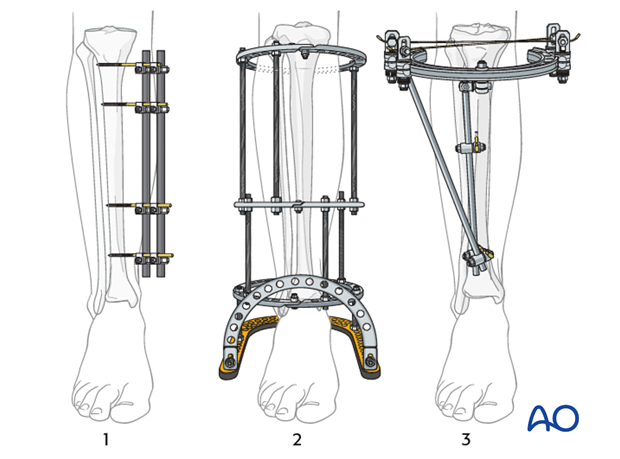
External fixation
In surgery for bone infection, external fixation may need to remain in situ for long periods. It may be necessary to replace one, or more, pins during the course of treatment.
There are 3 basic systems:
- external fixation with Schanz pins and tubular frames
- ring fixators anchored with tensioned wires
- hybrid ring fixators (using both tensioned wires and Schanz pins)
All three systems have advantages and disadvantages. The ring fixator frame is much more difficult to install, but can be used for compression and lengthening. They are also quite uncomfortable for the patient when ambulating. Hybrid frames are simpler and tensioned wires may have fewer pin-related problems, while external fixation with Schanz pins is the simplest and is very adaptable.
These frames must provide stability, just as in any other fracture fixation situation. If instability occurs (loosening, or infection) then they must be replaced.
Internal fixation with plates and nails
Plates and nails involve implantation into the site of the treated infection. They are rarely used in any previously infected wound as this increases the risk of infection recurrence.
Bony reconstruction
Eradication of infection, restoration of stability, and soft-tissue closure should be achieved before limb reconstruction.
At this stage, bone grafting, or bone transport, is performed, as needed, to achieve union, and/or to reconstruct a defect.
Initially, it may be helpful to accept some limb shortening to achieve wound closure, stability, and/or fracture healing. If the shortening is excessive, or if it involves angulation, these can be corrected with distraction histogenesis (Ilizarov technique), as a final stage of reconstruction.
Bone graft options
Autogenous cancellous bone graft, harvested from any standard donor site is the material of choice for promoting union and filling smaller defects.
For treating tibial fractures, posterolateral, or central placement, adjacent to healthy muscle, may avoid the infected focus. For the humerus, femur, or forearm, the best position of the graft depends on the defect, the soft-tissue envelope and the fixation.
Bone defects remaining after resection of dead, or infected, bone are challenging to treat. The longer the defect, the more difficult the treatment.
Circumferential defects of 1-6 cm in long bones usually heal if filled with autogenous bone graft, and stabilized appropriately. Defects greater than this usually need distraction osteogenesis, or free vascularized bone transfer.
Open cancellous bone grafting (Papineau technique), leaving the graft exposed beneath a non-adherent dressing, is a well-tried technique for reconstructing defects. It is best used for strengthening partial segmental defects. It can achieve bony bridging and secondary soft-tissue coverage concurrently, since granulation tissue should form over the graft and under the moist dressing. A split-thickness skin graft can then be applied.
Some of the superficial bone graft is inevitably lost and will have to be removed before granulation occurs. This technique has a fairly high reported success rate.
A more modern adaptation is to use a VAC over cancellous bone graft.
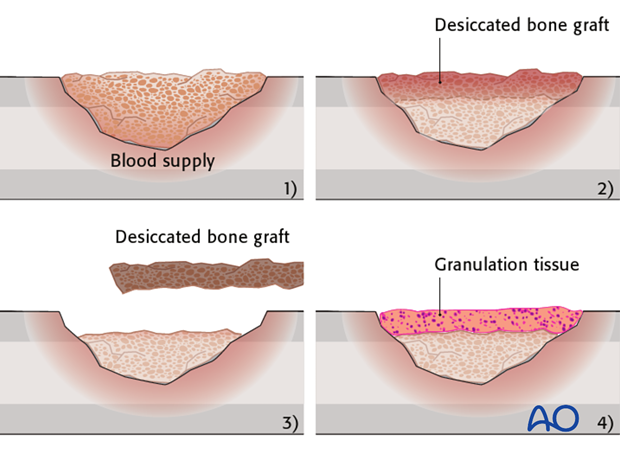
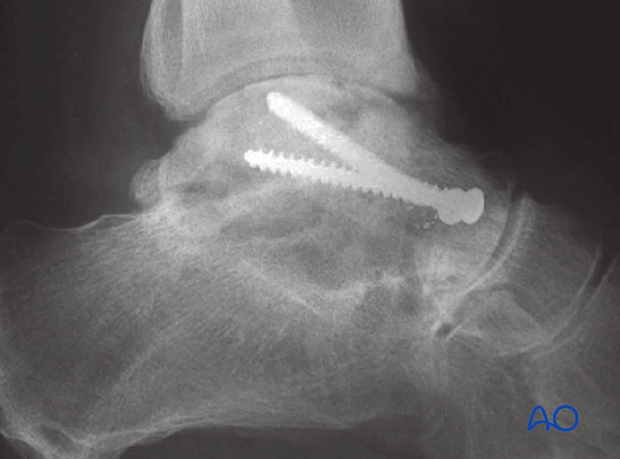
This case shows an infected subtalar fusion treated by Papineau technique, using vacuum assisted closure.
The case illustrations are taken from Archdeacon MT, Messerschmitt P (2006) Modern Papineau technique with vacuum-assisted closure. J Orthop Trauma; 20(2):134-7.

Healed soft tissue defect.

Underlying healed talus fracture.
Bone transport with distraction osteogenesis
Slow distraction of an osteotomy with stable (usually external) fixation creates new bone. Distraction rate is usually limited to 1 mm per day.
Soft-tissue reconstruction
Soft-tissue coverage
As a rule, soft-tissue coverage without complete surgical clearance of the underlying infection is useless.
A further rule is that wound closure under tension will always fail. The wound edges will die, the wound re-opens and secondary infection is unavoidable.
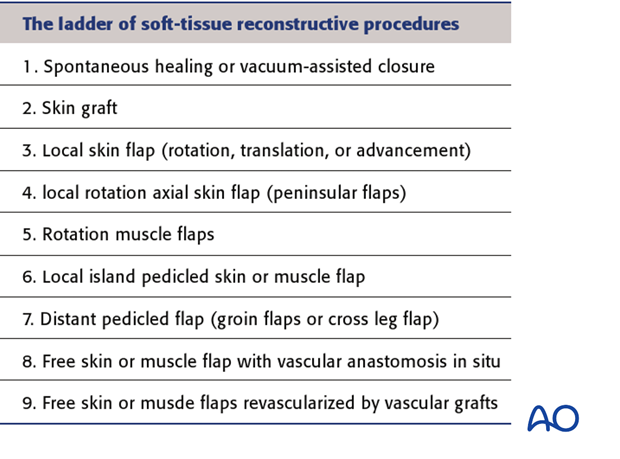
Direct suture closure is rarely possible, or desirable. Consider split-thickness skin grafts, rotational muscle flaps, fascio-cutaneous flaps, or free vascularized flaps.
Negative pressure dressings (NPWT) (vacuum-assisted closure (VAC)) are very useful over some open wounds, or open soft-tissue defects. As experience with these VACs is increasing, it seems that prolonged VAC usage (>10 days) should be avoided.
Split-thickness skin grafting and secondary wound healing
If an open wound involves loss of skin and subcutaneous tissue, but has a base of healthy muscle, fascia, or tendon sheath, granulation tissue will form on the base and a split-thickness skin graft (STSG) can be applied, or the wound can be allowed to heal in from its sides (second intention).
Bare bone (without periosteum), exposed blood vessels, nerves and tendons (without paratenon) are all harmed by desiccation and do not support granulation tissue and STSG. These tissues should never be left exposed, and should be kept moist with appropriate dressings. Alternative coverage techniques should be used. Definitive coverage should be achieved as soon as possible.
The “reconstructive ladder” shown on the left presents in increasing order of complexity the options available for wound closure, and is helpful for treatment planning.
Other than STSG and some local rotation flaps, the more complex soft-tissue reconstructions should be undertaken by surgeons experienced in these techniques, e.g., plastic surgeons.
9. Treatment - amputation
Amputation for osteomyelitis
It is rare for systemic infection to flare out of control in patients with chronic osteomyelitis. For such patients, amputation is almost never an urgent, life-or-death decision. However, should repeated attempts to control infection, secure bone healing and restore function be unsuccessful, amputation may prove to be the best way to restore function and help the patient to resume a more normal life.
The informed decision to amputate should be considered carefully and individually, including both the patient and family.
The surgeon’s job is to inform the patient about realistic expectations.
Different cultures, countries and religions bring different perspectives to this controversy. In many parts of the world, simple inexpensive but useful prosthesis can be made locally.
This illustration shows a basic below knee prosthesis from Africa and the celebrated Jaipur foot from India, each made locally.

If the patient makes the informed decision to proceed to amputation, the surgeon should plan the most functional level of amputation proximal to the diseased tissue. Consultation with a prosthetist may be helpful. The patient may wish to discuss amputation with another person who has undergone this procedure at a similar level.
The patient should attain optimal possible nutritional and physiological condition, with suppression of active infection by antibiotics, further surgical clearance, or even a preliminary amputation just above the infected zone.
Once all of the infected tissue has been amputated, continued infection treatment is no longer required.












