Heterotopic ossification
1. Introduction
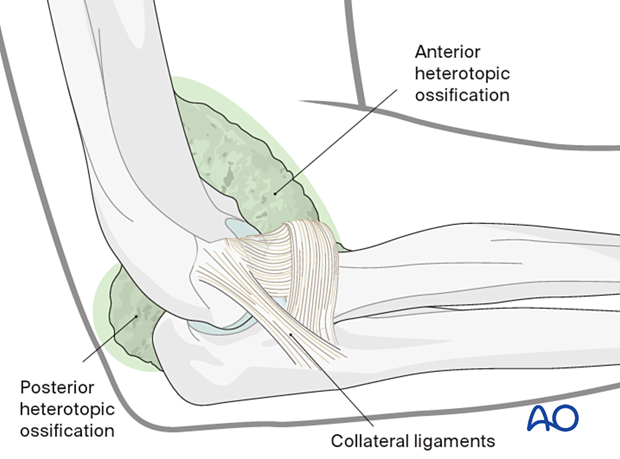
Formation of heterotopic bone can occur around the capsule and the ligaments or the muscle. It can also encase neurovascular structures.
It is a known sequela of elbow trauma, severe burns, or injury to the central nervous system. Severity ranges from minor clinically insignificant flecks of bone to complete bony ankylosis.

2. Etiology
Factors that contribute to heterotopic ossification include:
- Complexity of fracture or dislocation
- Extent of soft-tissue injury
- Surgical exposure and technique
- Possibly timing of surgery
- Associated injuries (CNS)
3. Diagnosis
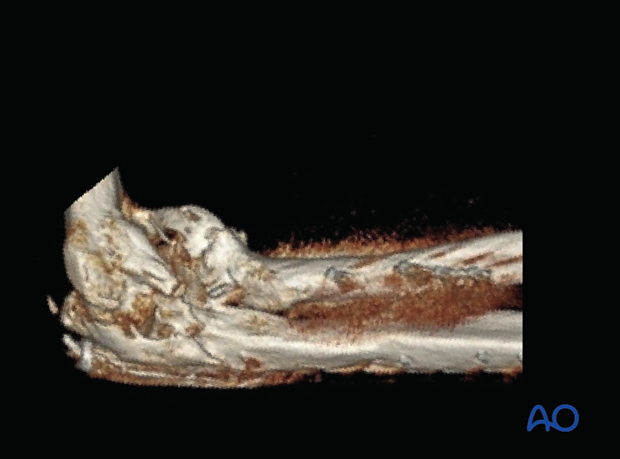
X-ray and 3D-CT imaging are essential to characterize the heterotopic ossification.
Preoperative electrodiagnostic testing is indicated with clinical findings of neuropathy.
Preoperative bone scan, erythrocyte sedimentation rate (ESR), or alkaline phosphatase measurements are of limited value in the diagnosis and management of heterotopic ossification.
Classification (Hastings) is based on location and/or functional impairment:
- Class I - No functional limitation
- Class II - Limitation in ≥ 1 plane
- Class III - Ankylosis
Subdivision for II and III:
- A (flex/ext)
- B (pro/sup)
- C (both)
4. Indication for surgical resection
Indications for surgery are:
- Functional impairment
- Progressive nerve deficit
The timing of surgery has been debated, but heterotopic bone should be mature on x-rays. Early (4–6 months) is better as the patient is more motivated, the bone is softer, and there is less muscle atrophy.
Relative contraindications are infection, nonunion, and poor motor control.
5. Skin incision
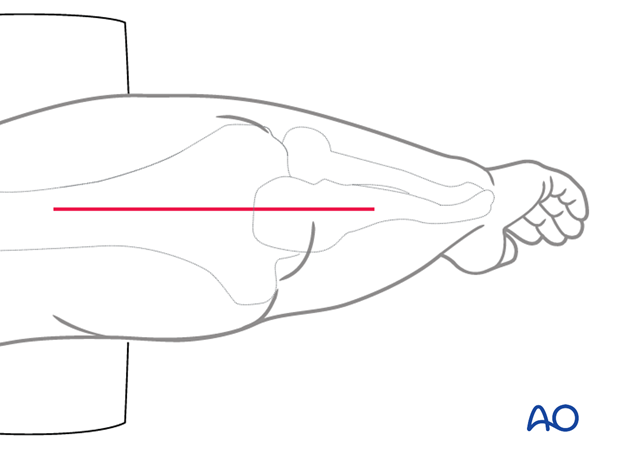
The approach is dependent on the location of the heterotopic bone. Take into account previous incisions or skin quality.
The posterior exposure permits an approach to the posterior aspect of the elbow. By epifascial dissection, it also allows exposure of the lateral and medial aspects of the elbow.
6. Posterior procedure
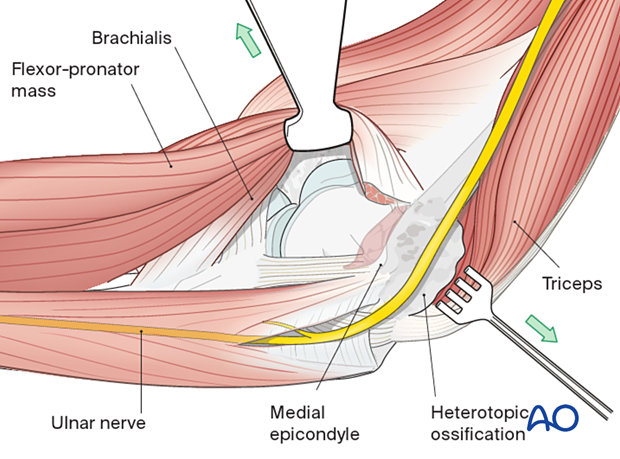
Heterotopic ossification around the ulnar nerve
Identify the ulnar nerve first (preoperative CT and previous op-notes should be scrutinized for details of location of ulnar nerve) as the nerve may be encased in bone, particularly with heterotopic ossification associated with severe burns.
It is often safest to locate the nerve proximally and then trace it distally.
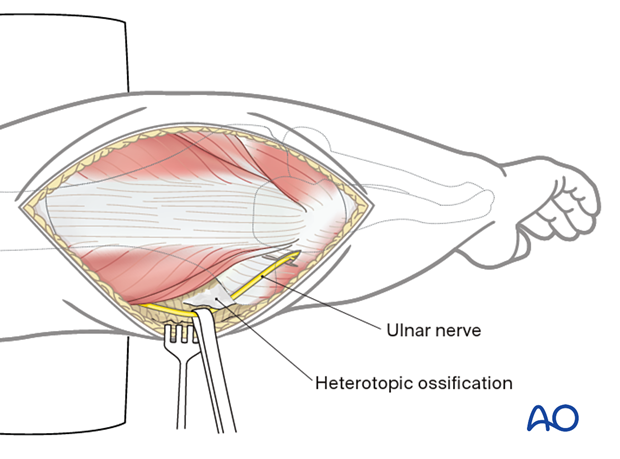
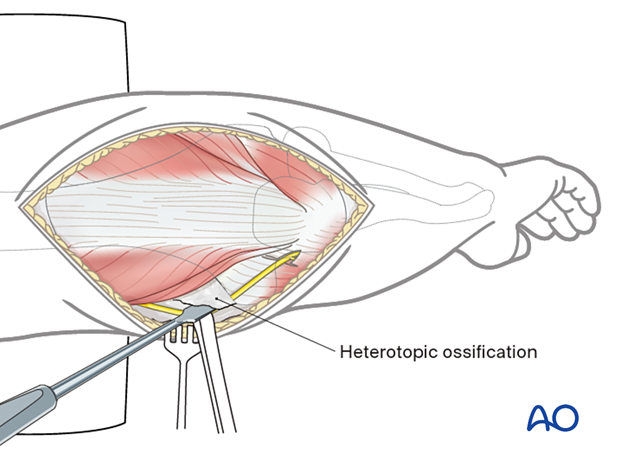
Excess bone around the nerve can be removed by sharp dissection and with a rongeur or small osteotome.
Heterotopic ossification in the olecranon fossa
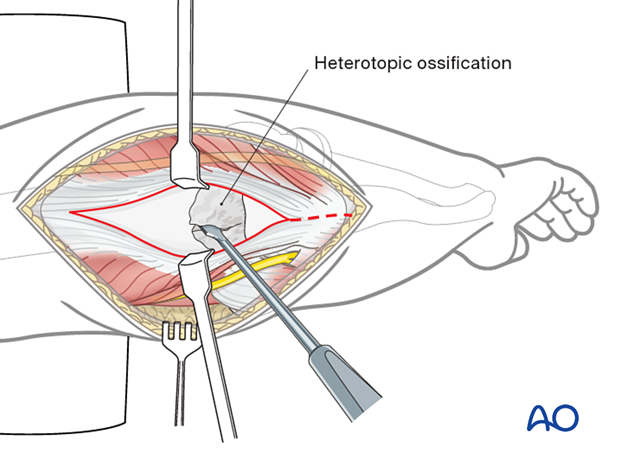
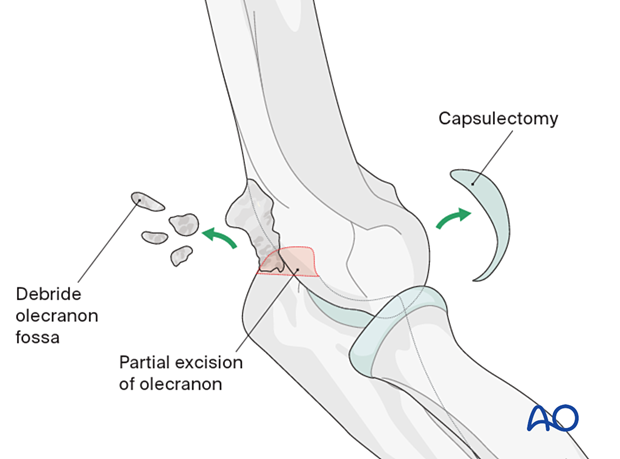
Heterotopic ossification in the olecranon fossa may be approached through a triceps-split approach.
Remove the bone with a rongeur, osteotome, or high-speed burr.
An olecranon-tip excision may be helpful.
Once the olecranon fossa is cleared, create an aperture in the humerus with a high-speed burr to allow removal of heterotopic bone from the anterior compartment of the joint (Outerbridge-Kashiwagi procedure).
7. Lateral column procedure
Use the posterior exposure and lateral epifascial dissection to approach the lateral column.
If there is any chance the radial nerve or posterior interosseous nerve (PIN) are at risk, they need to be identified.
The extensor carpi radialis longus and brevis of the humerus, along with brachioradialis, are elevated.
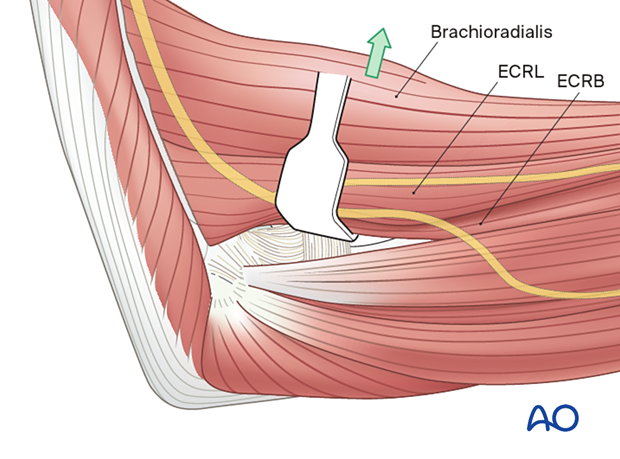
Open the interval between extensor carpi radialis brevis and extensor digitorum communis. The lateral collateral ligament should be spared.
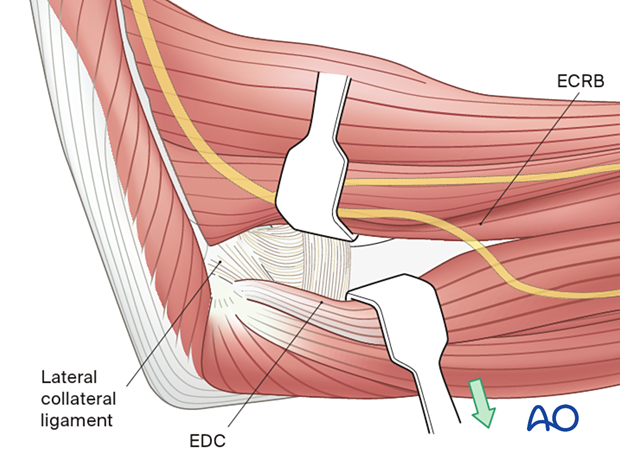
Posterior to the lateral ligament, the triceps and anconeus are elevated off of the distal humerus and ulna, respectively.
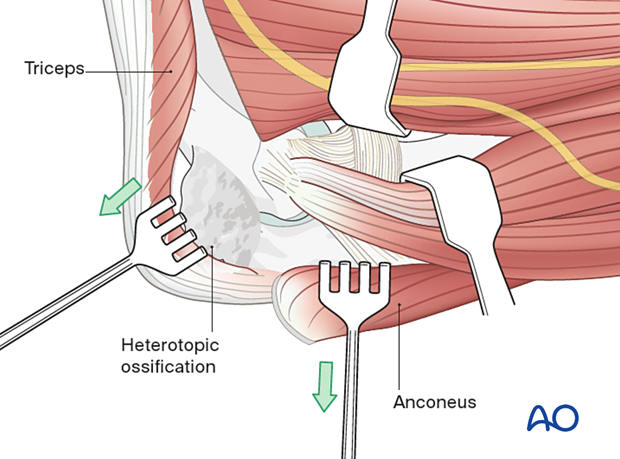
This approach will allow a capsulectomy and debridement of the coronoid fossa, olecranon tip, and olecranon fossa.
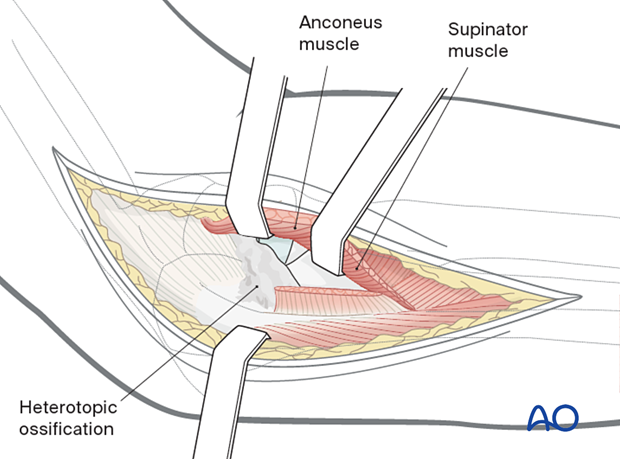
Heterotopic bone between the radius and ulna (or even synostosis) can be resected using the Boyd approach elevating the extensor carpi ulnaris and supinator of the ulna.
8. Medial column procedure
Use the posterior exposure and medial epifascial dissection to approach the medial column.
The over-the-top approach elevates the brachialis muscle off the distal humerus along with the anterior half of the flexor-pronator mass that is divided horizontally.
The anterior band of the medial collateral ligament (MCL) should be preserved, whereas the posterior and transverse band of the MCL can be excised if needed.
Posteriorly, the triceps is elevated off the distal humerus.
9. Confirmation of restoration of motion
Once heterotopic bone is removed, the elbow is gently mobilized to confirm restoration of motion.
It is safer to leave all implants from osteosynthesis in place until manipulation is completed.
If motion is still limited, reassess adequacy of bone excision or consider additional soft-tissue release (rarely the case).
Be mindful of postoperative elbow instability and be prepared for ligament reconstruction.
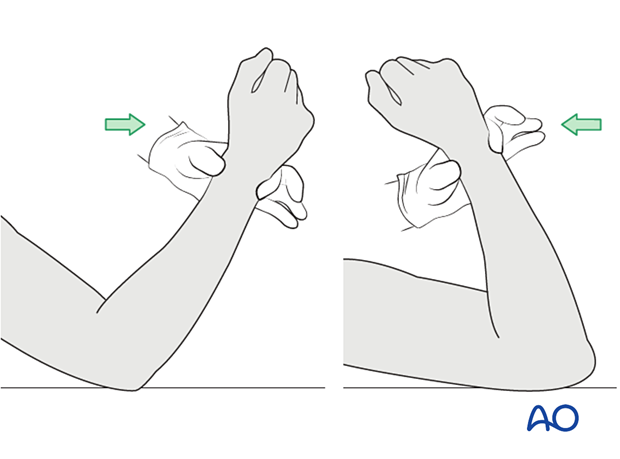
10. Aftercare
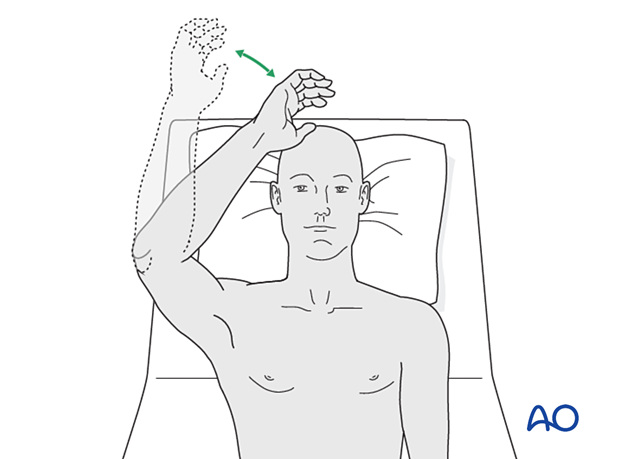
Active, self-assisted or gravity-assisted range-of-motion exercise is started immediately. The use of a continuous-passive-motion machine (CPM) is optional.
The use of NSAID, glucocorticoids, and radiation should be individualized.
The evidence for these treatments is inconclusive.