Intramedullary K-wire fixation
1. General considerations
Extraarticular fractures of the metacarpal neck may be stabilized with intramedullary K-wire fixation.
The K-wires are inserted through a small incision at the base of the metacarpal into the bone.
The stabilization principle follows a three-point bone support. This corrects the angulation of the head, controls the rotation, and avoids shortening.
AO teaching video
Metacarpal V, neck—Subcapital and comminuted fractures—Intramedullary splinting with two 1.25 K-wires
2. Patient preparation
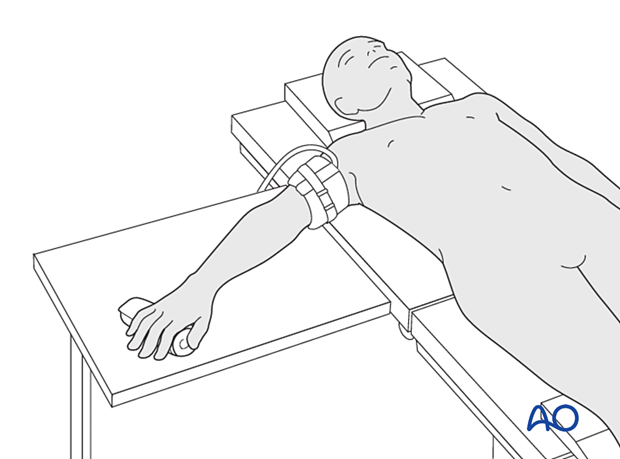
Place the patient supine with the arm on a radiolucent hand table.
3. Creating an entry portal
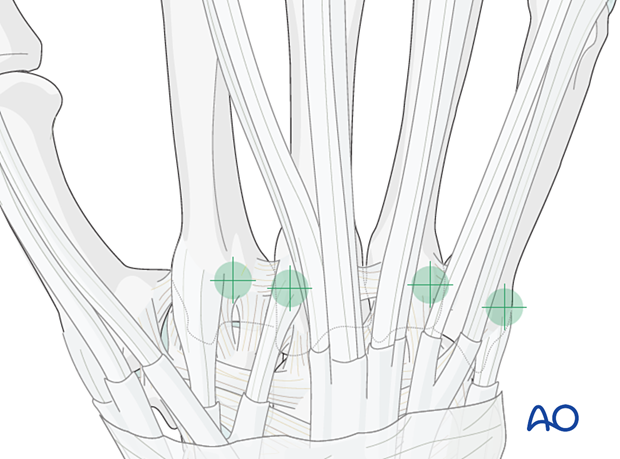
Location of the entry point
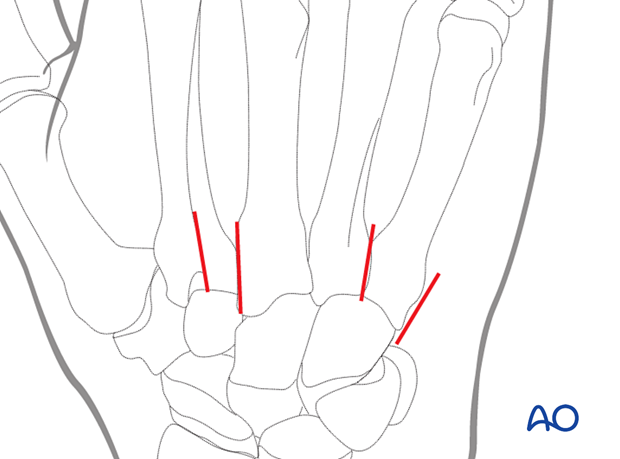
For the 5th metacarpal, the entry point is dorsoulnar at the metacarpal base without damaging the carpometacarpal joint and respecting the insertion of the extensor carpi ulnaris tendon. Check under image intensification.
For the other metacarpals, the entry point is dorsally at the metacarpal base. Take care so that the protruding ends of the K-wires will not interfere with the gliding of the extensor tendons.
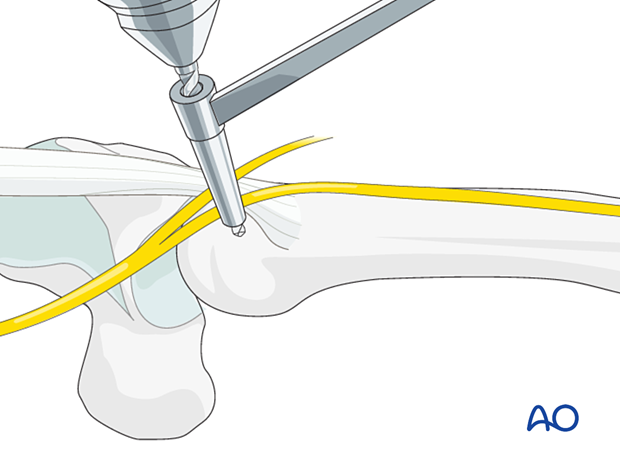
Skin incision
Perform a small longitudinal skin incision to allow drilling with a drill guide to protect the soft tissues.
Opening the cortex
Open the dorsoulnar cortex with a 2 mm drill bit. Start drilling perpendicular to the bone surface, so the drill does not accidentally slip off the bone.
A drill sleeve must be used to protect the dorsal sensory branch of the ulnar nerve or the extensor tendons.
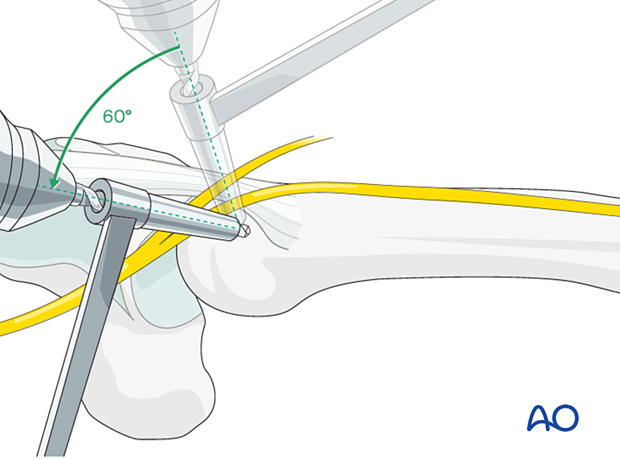
Preparing the entry portal
Tilt the drill by approximately 60°, so it enters the intramedullary canal at as obtuse an angle as possible.
Do not drill through the opposite cortex.
In this oblique direction, the drill hole is then enlarged with a 2.7 mm, or 3.2 mm, drill bit, or a burr.
4. Fixation
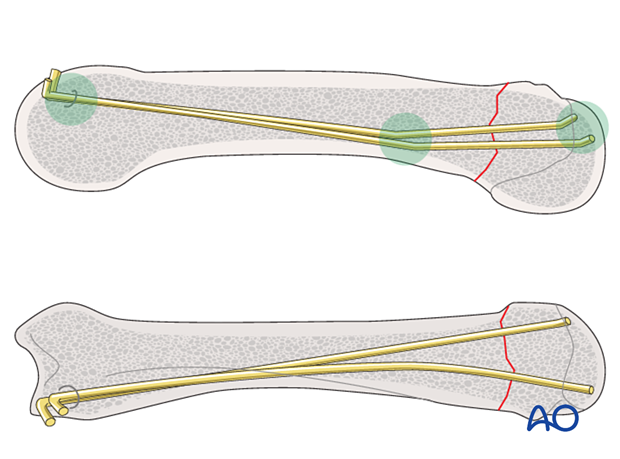
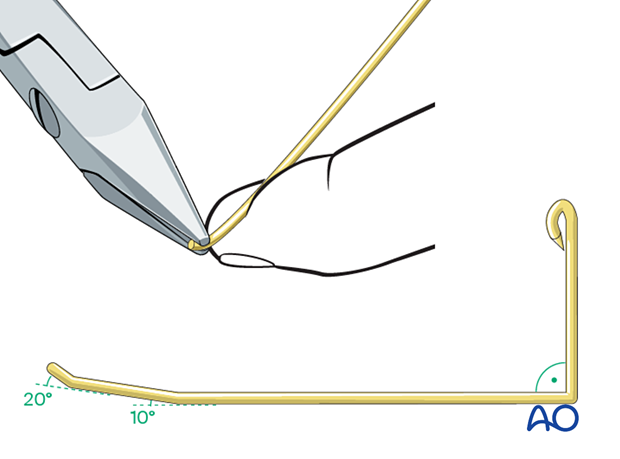
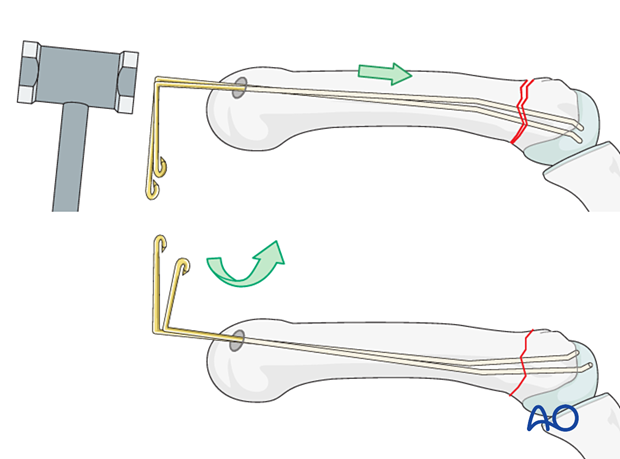
Prebending the K-wires
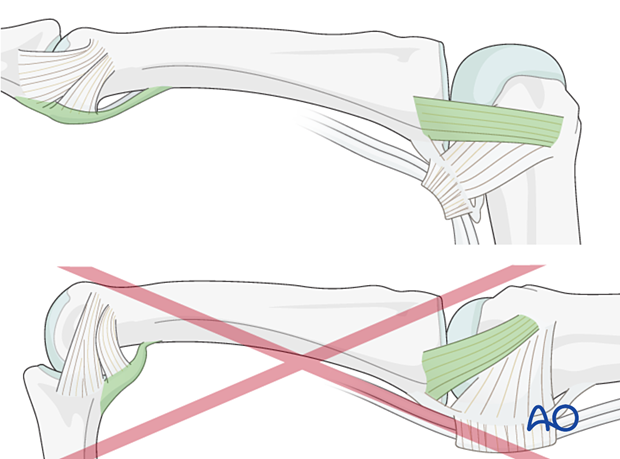
Two or three K-wires of 1 or 1.25 mm diameter have to be inserted with the blunt tip first to reduce the risk of perforating the thin cortex of the metacarpal head.
They are bent in the following way.
The distal tip is bent upwards with pliers by about 20°. About 2 cm further, the wire is bent in the same direction by not more than 10°.
At the point where the wire is slightly longer than the metacarpal into which it will be inserted, the proximal end of the wire is bent through 90° in the same plane. This way, the direction of the insertion can always be controlled.
To avoid injury, the sharp end of the wire is bent over.
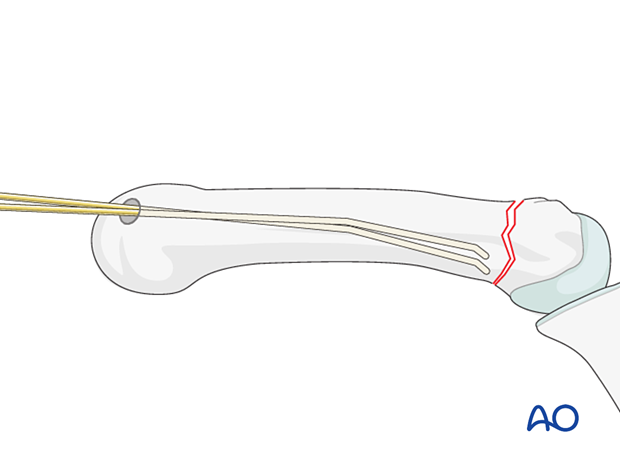
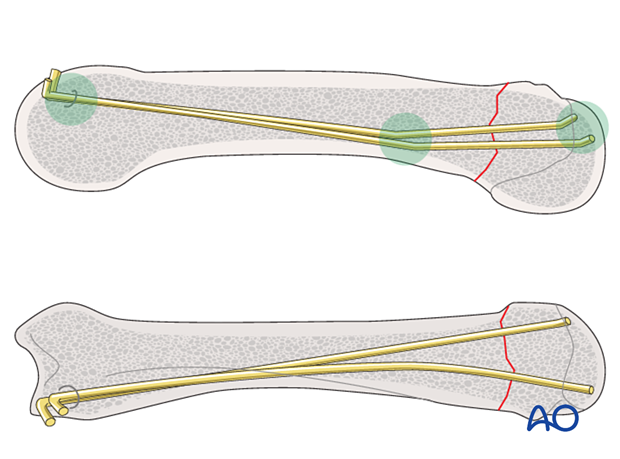
Wire insertion
Insert two wires manually into the medullary canal and advance them into the diaphysis without reaching the fracture zone. The bent tips should point in a palmar direction.
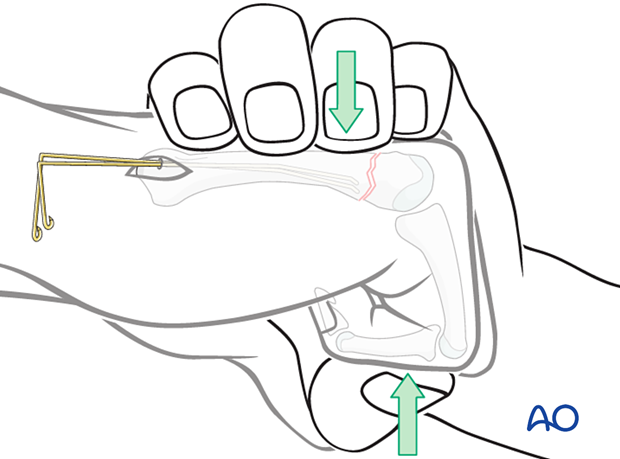
Preliminary reduction
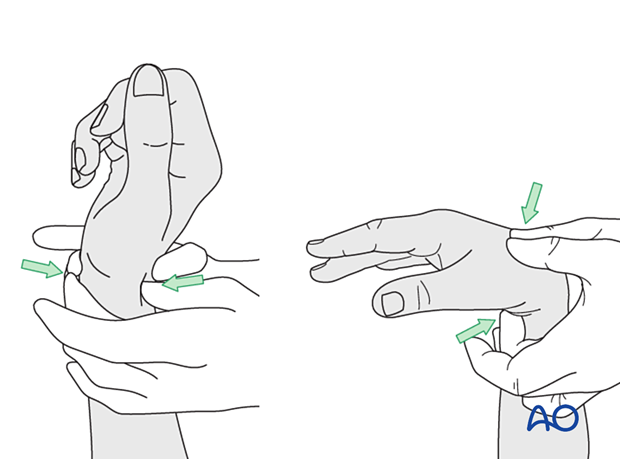
Reduce the fracture preliminarily by flexing the metacarpophalangeal (MCP) and proximal interphalangeal (PIP) joints to 90° and using the proximal phalanx to push up the metacarpal head (Jahss maneuver).
Reduction with K-wires
Advance the wires manually or with a hammer across the fracture zone into the head.
Confirm the correct position with an image intensifier. Ensure not to perforate the thin cortex.
Then rotate the K-wires so that the bent tips point dorsally and diverge in slightly different directions (dorsoradial and dorsoulnar).
Ideally, the blunt tips lie underneath the dorsal cortex of the head.
Confirm correct rotational alignment of the finger.
Complete fixation
This allows for a three-point fixation which increases the construct stability and prevents the K-wires from backing out proximally.
Then bend the K-wires at the level of the entry portal and cut them.
The ends of the K-wires may be buried under the skin or protruding from the skin. The latter will avoid a second surgery for K-wire removal but bears the risk of skin problems.
5. Checking alignment
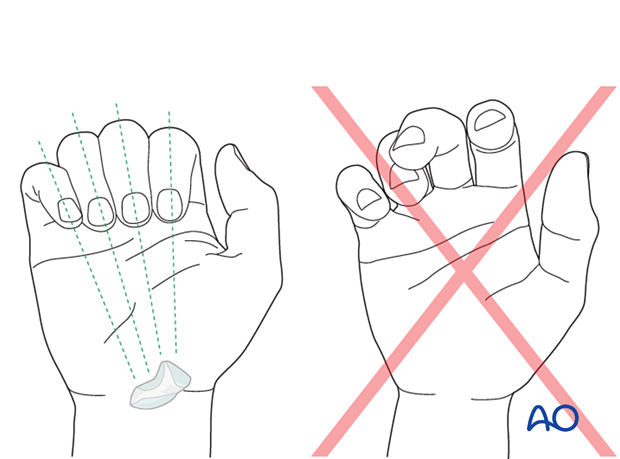
Identifying malrotation
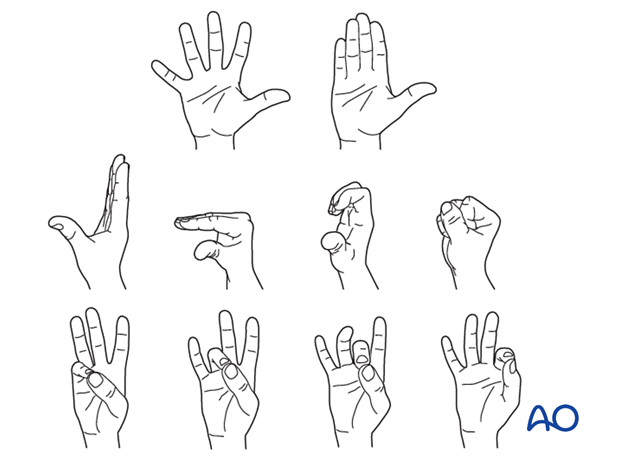
At this stage, it is advisable to check the alignment and rotational correction by moving the finger through a range of motion.
Rotational alignment can only be judged with flexed metacarpophalangeal (MCP) joints. The fingertips should all point to the scaphoid.
Malrotation may manifest by an overlap of the flexed finger over its neighbor. Subtle rotational malalignments can often be judged by a tilt of the leading edge of the fingernail when the fingers are viewed end-on.
If the patient is conscious and the regional anesthesia still allows active movement, the patient can be asked to extend and flex the finger.
Any malrotation is corrected by direct manipulation and later fixed. Flexing the MCP joints while preventing overlap of the fingers will reduce rotational displacement.
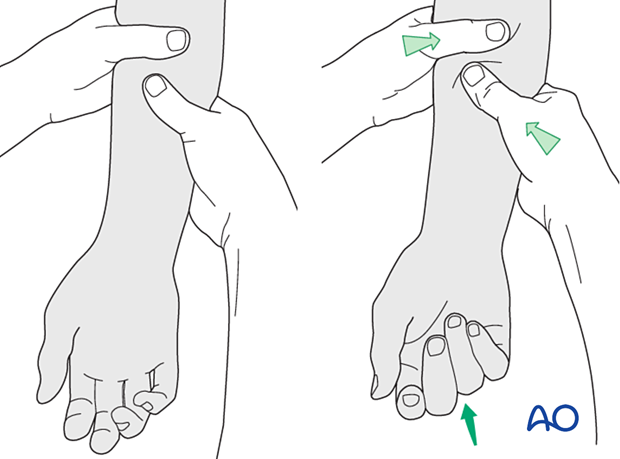
Using the tenodesis effect when under anesthesia
Under general anesthesia, the tenodesis effect is used, with the surgeon fully flexing the wrist to produce extension of the fingers and fully extending the wrist to cause flexion of the fingers.
Alternatively, the surgeon can exert pressure against the muscle bellies of the proximal forearm to cause passive flexion of the fingers.
6. Final assessment
Confirm anatomical reduction and correct placement of implants in AP, lateral, and oblique views.
7. Aftercare
Postoperative phases
The aftercare can be divided into four phases of healing:
- Inflammatory phase (week 1–3)
- Early repair phase (week 4–6)
- Late repair and early tissue remodeling phase (week 7–12)
- Remodeling and reintegration phase (week 13 onwards)
Full details on each phase can be found here.
Postoperative treatment
If there is swelling, the hand is supported with a dorsal splint for a week. This would allow for finger movement and help with pain and edema control. The arm should be actively elevated to help reduce the swelling.
The hand should be splinted in an intrinsic plus (Edinburgh) position:
- Neutral wrist position or up to 15° extension
- Metacarpophalangeal (MCP) joint in 90° flexion
- Proximal interphalangeal (PIP) joint in extension
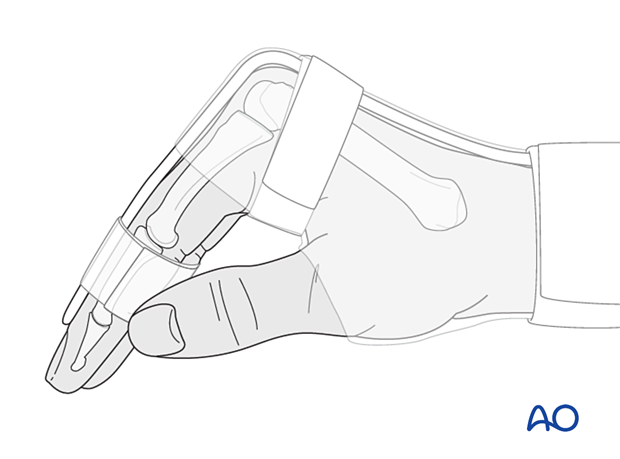
The reason for splinting the MCP joint in flexion is to maintain its collateral ligament at maximal length, avoiding scar contraction.
PIP joint extension in this position also maintains the length of the volar plate.
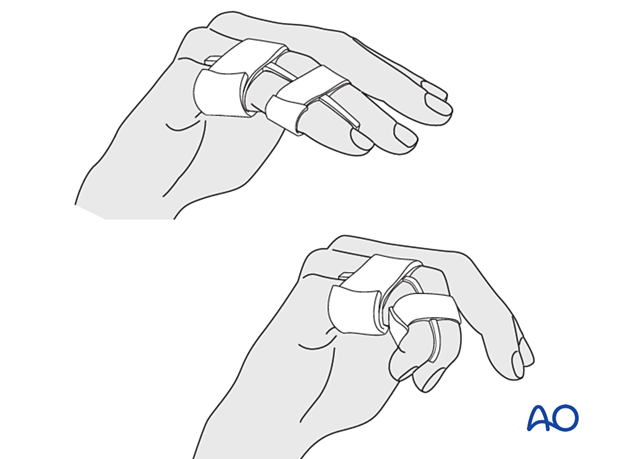
After subsided swelling, protect the digit with buddy strapping to a neighboring finger to neutralize lateral forces on the finger.
Functional exercises
To prevent joint stiffness, the patient should be instructed to begin active motion (flexion and extension) immediately after surgery.
Follow-up
See patient after 2 days for changing of the dressing. After 10–12 days, remove the sutures and confirm with x-rays that no secondary displacement has occurred.
At that time, active mobilization is started, supervised by a physiotherapist. The splint is continued.
Additional x-rays are taken 6 weeks after internal fixation to confirm fracture consolidation. Usually, the K-wires can then be removed.












