Lumbar endoscopic unilateral laminotomy for bilateral decompression (LE-ULBD)
1. Introduction
This procedure is analogous to the microscopic tubular procedure, though working through a smaller working channel.
The interpedicular distance increases moving caudally in the lumbar spine. Different endoscope diameters are available for this procedure. It is important not to use the larger endoscope at the cranial levels to avoid excessive facet resection.
2. Required instruments
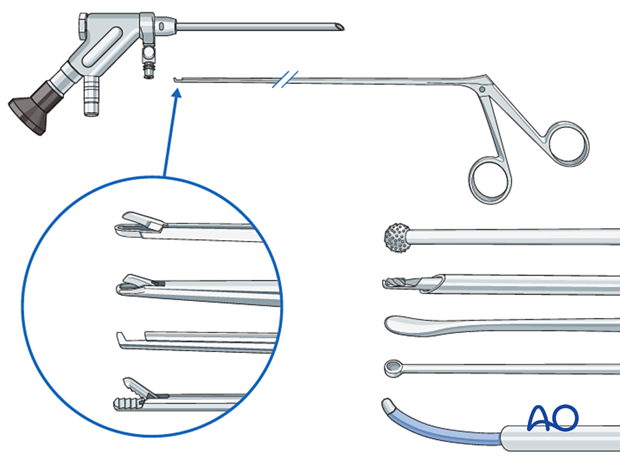
The following specialized instruments are recommended for this procedure:
- Endoscopy cart (video, irrigation pump (50 mmHg), radiofrequency unit, drill)
- Interlaminar endoscope
- Blunt dissector
- Micro-punch
- Grasping forceps
- Kerrison rongeur
- Curette
- Bipolar coagulator
- Burr
- C-arm
3. OR set up and patient positioning
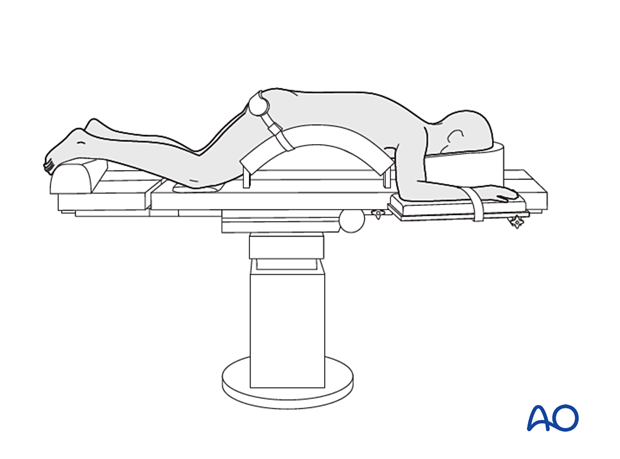
The patient is placed prone on a Wilson frame or with pelvic and thoracic rolls.
4. Positioning of C-arm
In the AP view, adjust the C-arm until:
- the endplate of the caudal level is straight
- the spinous process is centered on the disc space
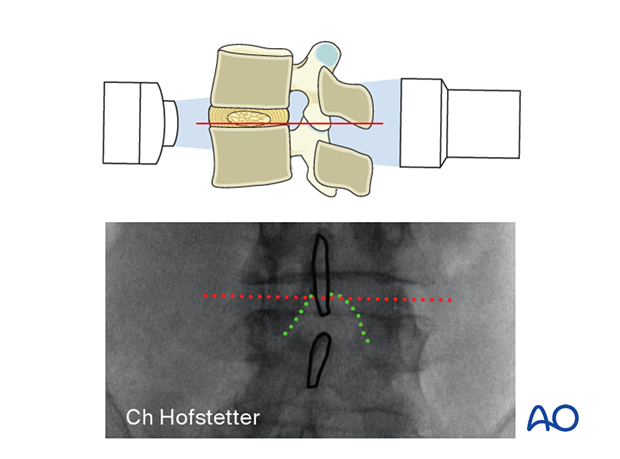
To obtain the largest window between the cranial and caudal lamina, tilt the C-arm to add 0°–5° of kyphosis for the upper lumbar levels and 10°–15° of kyphosis for the lower lumbar levels.
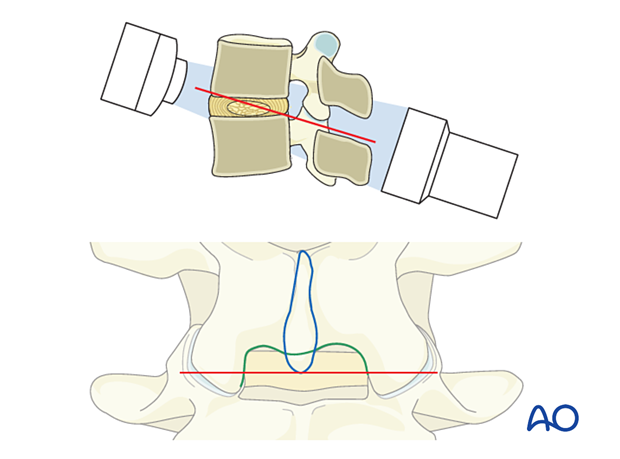
Optimizing the approach corridor to the lateral recess will minimize the need for bone resection.
5. Visualization of the surgical field
Incision
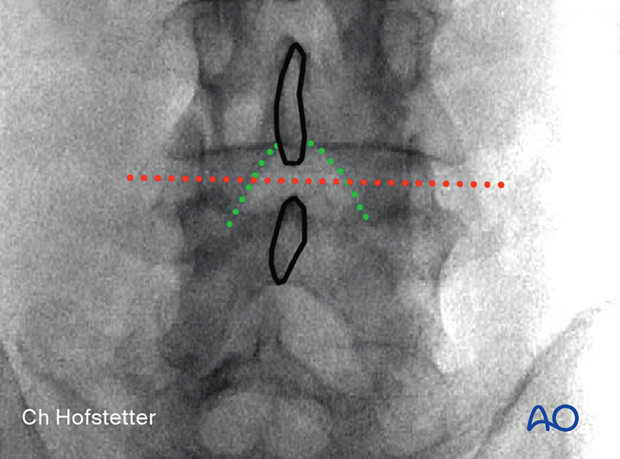
Use AP intraoperative imaging to identify the inferior medial edge of the cranial level on the ipsilateral side.
The incision line is marked at this line, centered over the disc.
The skin may be infiltrated as per the surgeon’s preference.
Use an 11-blade scalpel to make a 1 cm incision through the skin and lumbar fascia.
Insertion of dilators
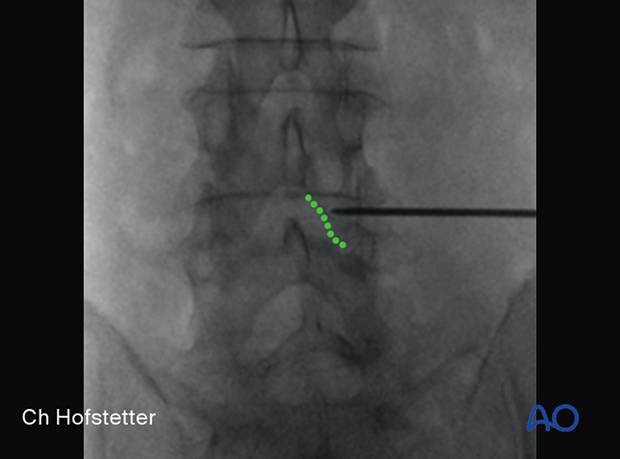
Insert the first dilator, angle it slightly medially, and “feel” for the spinous process and lamina base. The goal is to reach the inferomedial laminar edge.
After the first dilator has been positioned correctly onto bone, verify that it is located at the correct level using fluoroscopy.
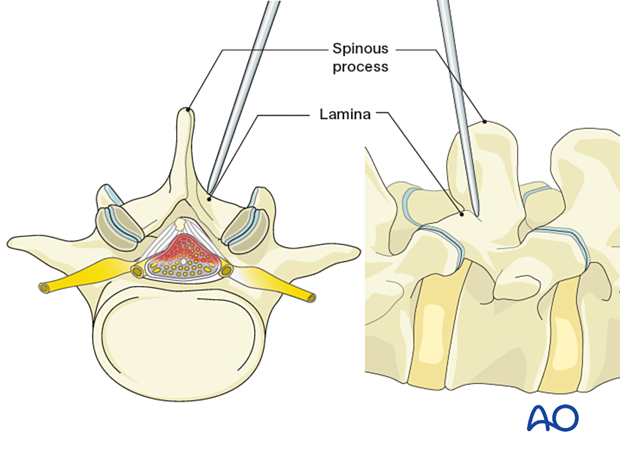
Insert sequential dilators onto the inferomedial lamina edge.
Palpate to ensure that the dilators are docked on bone at all times.
Once the desired dilation is achieved, ensure that the bevel of the working channel is facing medially. This will reduce the risk of dural injury if the working channel slips.
Use an x-ray to verify the correct position of the working channel in the AP and lateral view.
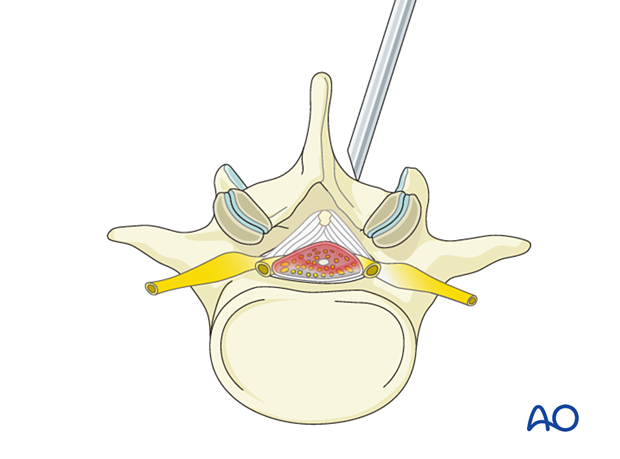
Visualization
Insert the endoscope into the working channel.
Use the bipolar coagulator and pituitary rongeurs to dissect tissue and identify the ligamentum flavum and the inferior medial edge of the lamina.
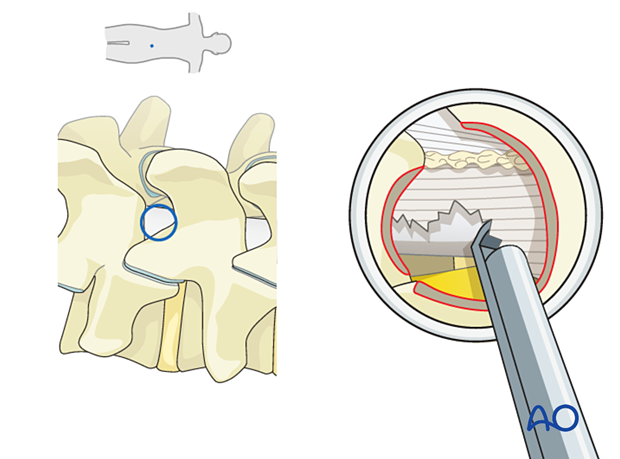
Cranial laminotomy
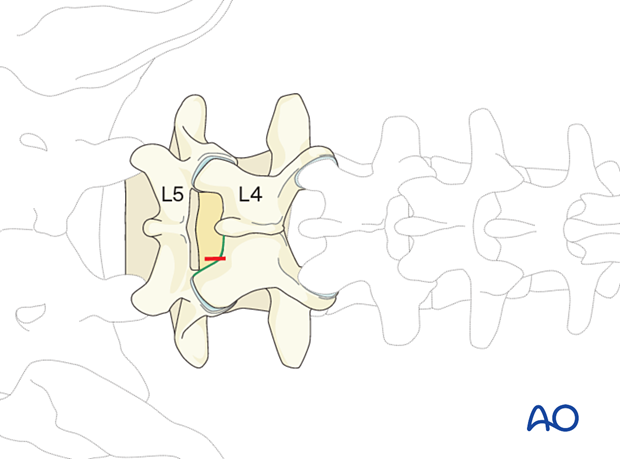
Identify the interface of the ligamentum flavum and the inferior medial edge of the cranial lamina.
Start drilling the inferior edge of the cranial lamina, moving along the edge of the lamina from lateral to medial in a cranial direction.
As the drilling proceeds cranially, care must be taken as there may not be underlying ligamentum flavum protecting the dura at its insertion.
As you move medially, you will undercut the base of the spinous process.
Undercut the contralateral lamina along the insertion of the ligamentum flavum. Proceed until the contralateral lateral recess is reached.
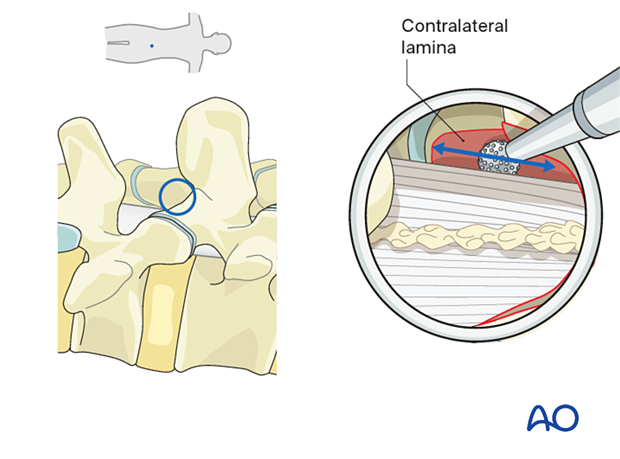
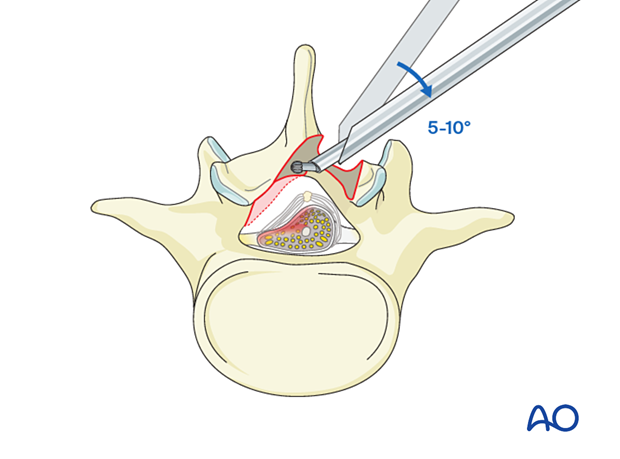
The working channel may have to be angled 5°–10° medially to facilitate contralateral decompression.
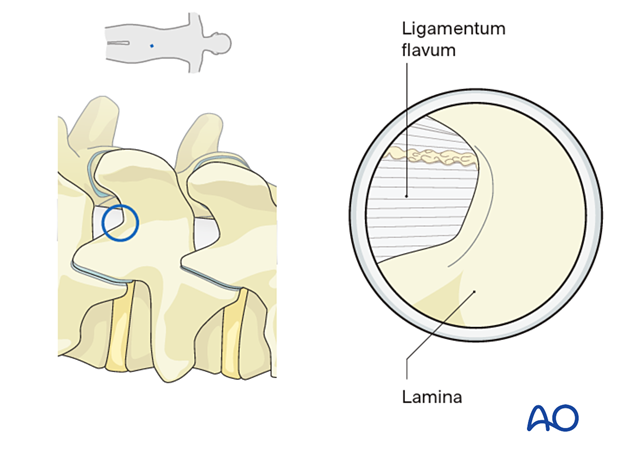
Caudal laminotomy
Start drilling laterally and move along the edge medially.
Identify the interface of the ligamentum flavum (LF) and the superior medial edge of the caudal lamina.
The contralateral superior edge of the caudal lamina is also drilled down to the LF.
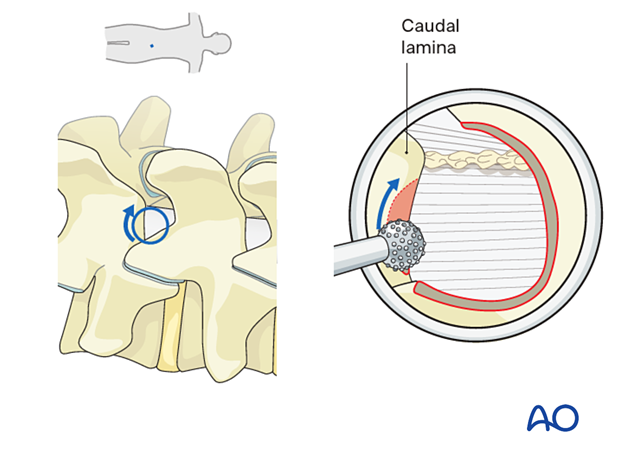
As the drilling proceeds caudally, care must be taken as there may not be underlying ligamentum flavum protecting the dura.
6. Enter the epidural space
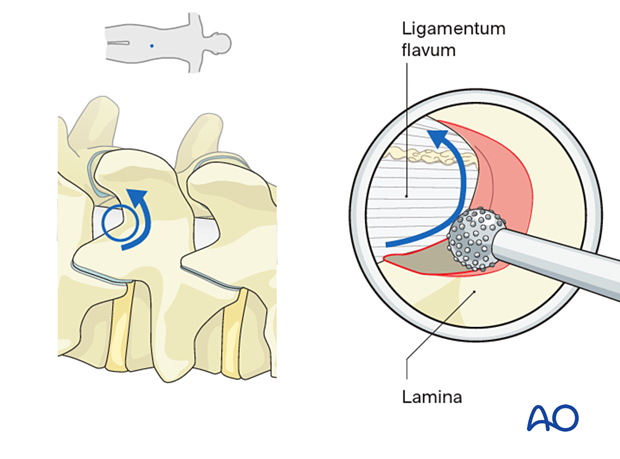
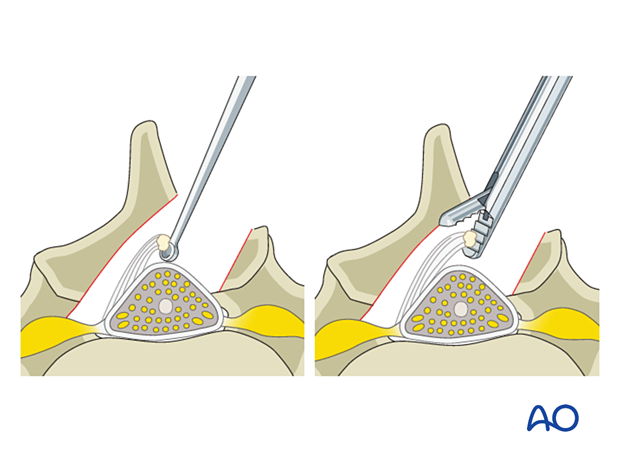
Flavectomy
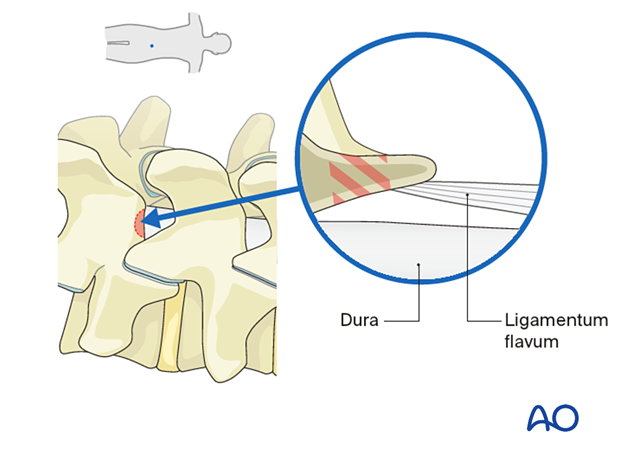
Once the bony decompression is complete, the ligamentum should be visualized.
Detach the ligamentum flavum from the remaining bony edges and the cranial and caudal insertion points using a curette or a Kerrison rongeur.
Once the ligament is circumferentially freed, use grasping forceps to resect the ligament, moving in a caudal to cranial direction.
In elderly patients, those with long-standing high-grade stenosis or calcified ligaments, the ligament may be adherent to the dura. Dissection beneath the ligamentum to define a plane with the dissection may be required to prevent dural tears during the resection of the ligamentum.
Lateral recess decompression
Additional bony decompression of the medial aspect of the superior articular process (SAP) on the ipsilateral or contralateral side using Kerrison rongeurs or a side-biting burr can be performed at this stage to achieve adequate decompression of the traversing nerve root.
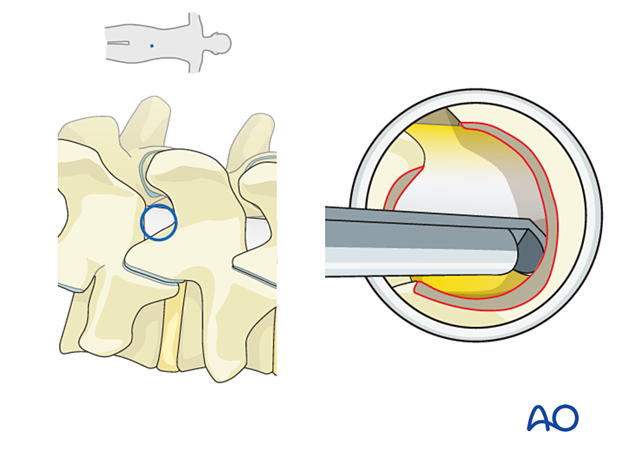
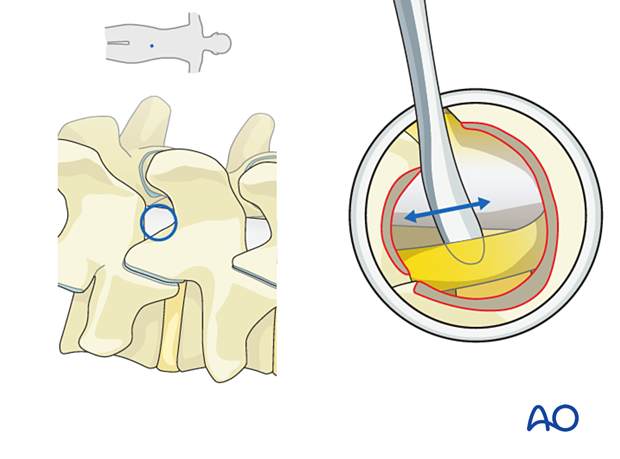
Mobilization of neural elements
Use a blunt dissector to verify that the lateral margins of the neural elements on the ipsilateral and contralateral sides are easily mobilized.
7. Endoscope removal and closure
Hemostasis is achieved with hemostatic agents or bipolar cautery.
The endoscope is removed, and a deep dermal stitch can be placed at the surgeon’s discretion. A subcuticular stitch is used to close the skin.
8. Aftercare
The patient can usually be discharged on the day of surgery or the following day with a short course of pain medication and muscle relaxants.
Lumbar immobilization is not required.
Patients may feel incisional or muscular pain that usually subsides within a few days.
Patients can develop postoperative pain and muscle spasms in a delayed fashion.
If a dural tear occurs, no repair and bedrest may be sufficient for small tears, while larger tears and tears with extrusion of nerve roots may require fibrin sealant and an inlay graft. Sometimes conversion to open or tubular surgery with direct repair of the dura may be necessary.












