Lag screw with or without neutralization plate
1. Introduction
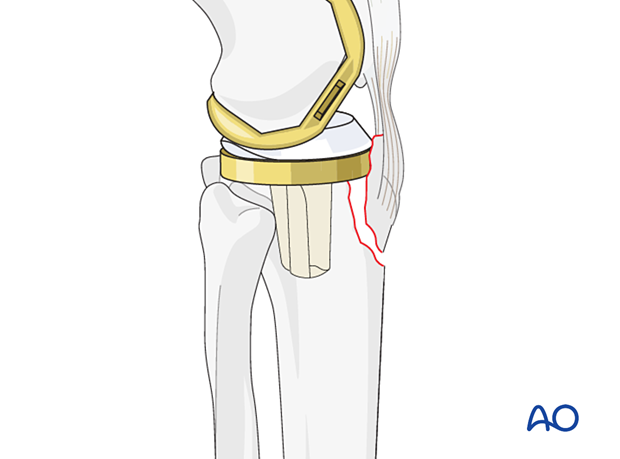
The stabilization of periprosthetic fractures that disrupt the extensor mechanism at the tibial tubercle is critically important to knee function.
Fixation is challenged by the size of the fracture fragment, and the need for expeditious mobilization of the knee.
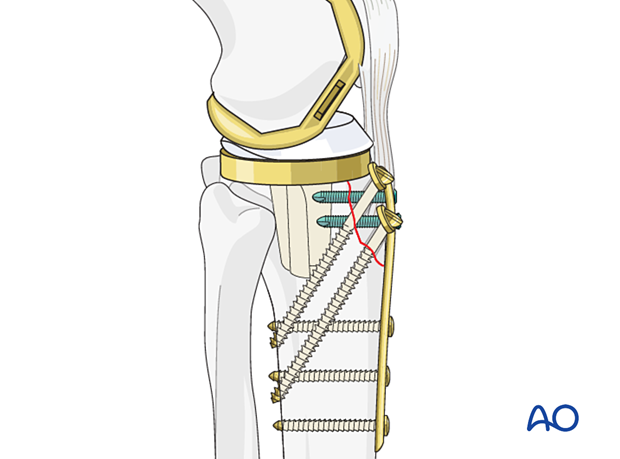
Neutralization for large fragments
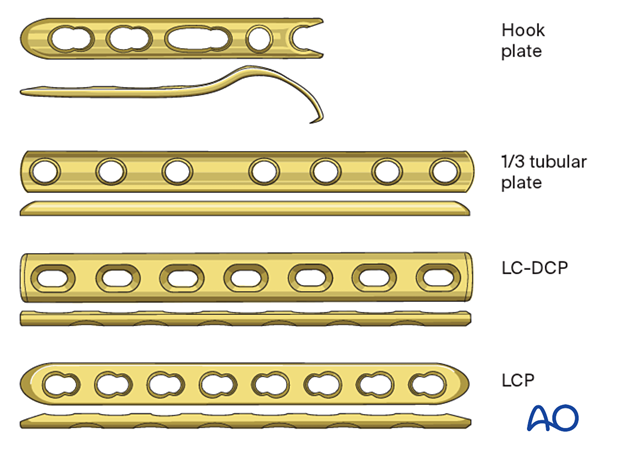
If fracture fragment size allows for neutralization, a small fragment plate is typically utilized. This may be inclusive of locking fixation if desired.
A hook plate is helpful with a smaller non-comminuted fragment. An interfragmentary compression screw is inserted through the plate.
2. Patient preparation and approach
In most cases, the midline approach to the knee that was used for the knee arthroplasty will be extended in order to adequately expose the fracture.
The obliquity of the fracture will dictate a medial, anterolateral (open or minimally invasive approach), or posteromedial extension to the prior incision.
Small incisions may be made over the distal aspect of the plate utilizing fluoroscopy as a guide, in order to minimize larger surgical approaches.
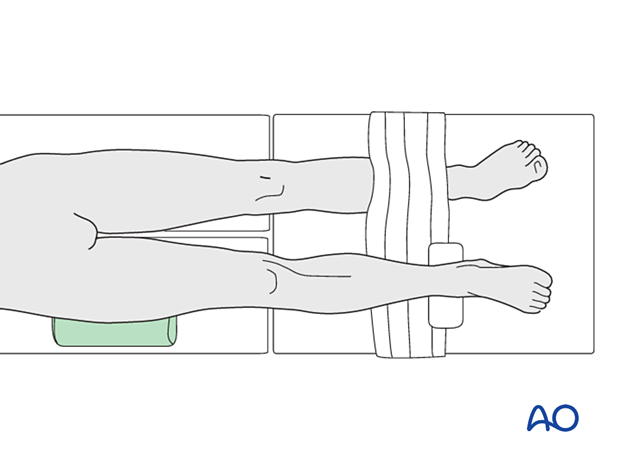
With rare exceptions, supine positioning with a bump under the ipsilateral greater trochanter will achieve neutral rotation of the limb.
Positioning the limb in full extension will facilitate the reduction of the tibial tubercle and decrease deforming forces across the fixation construct.
3. Reduction
The fracture site should be exposed, cleared of hematoma and debris, and reduced utilizing direct reduction methods.
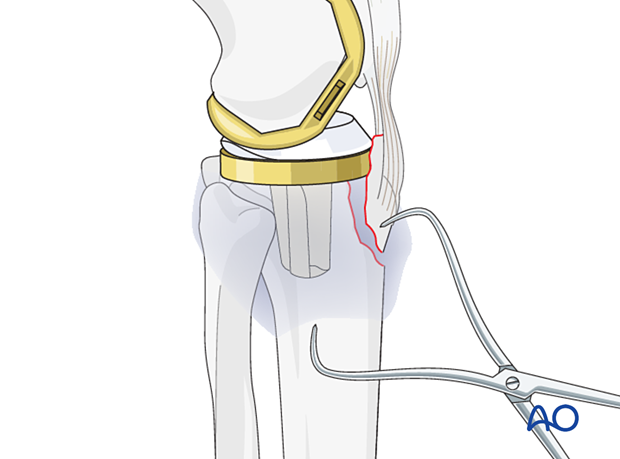
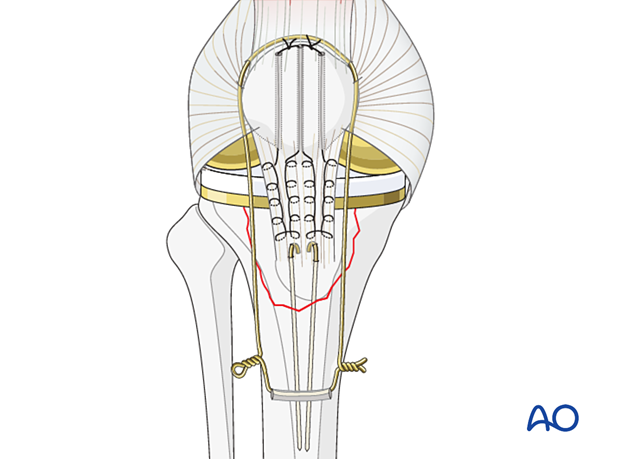
Large non-absorbable sutures can be inserted in the patellar tendon to aid in reduction.
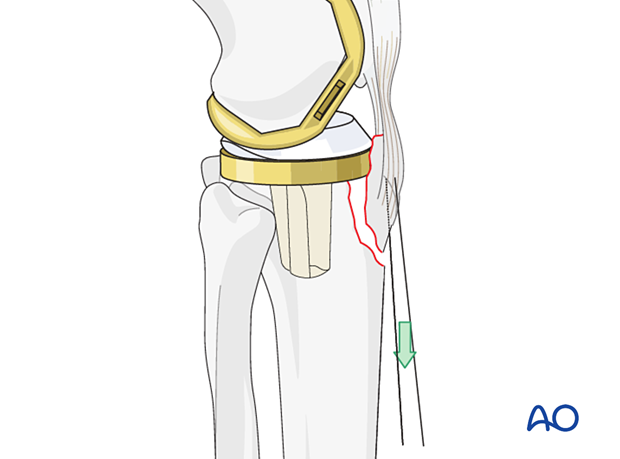
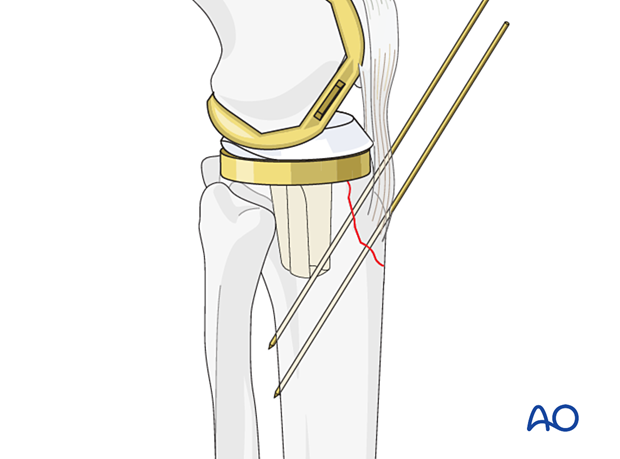
Provisional fixation is attained with K-wires.
4. Fixation
Lag screw fixation
Bicortical lag screws are inserted according to the standard technique. If the fracture fragment will allow for multiple lag screws, they should be inserted in a divergent pattern.
The screws can be countersunk to avoid soft tissue prominence. Washers can be utilized to disperse forces more evenly in the near cortex.
Lag screws should not be inserted through the cement mantle as reliable compression cannot be achieved.
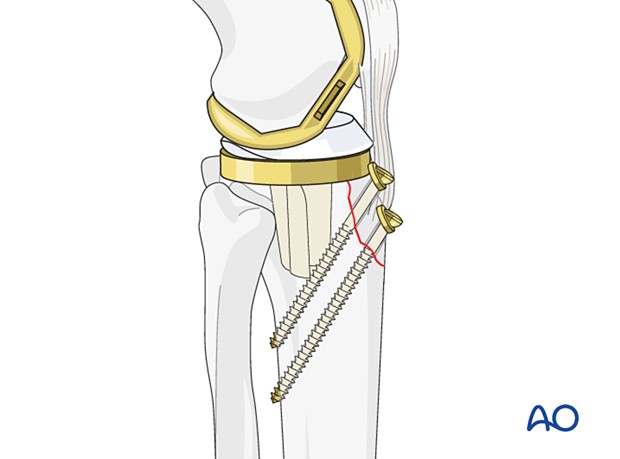
Plate contouring
In order to achieve earlier mobilization, the addition of a neutralization plate may reinforce the construct. The surgeon should ensure that the plate selected is perfectly contoured to the bone as not to disrupt the compression that is achieved by the lag screw. The plate should be positioned to avoid plate prominence.
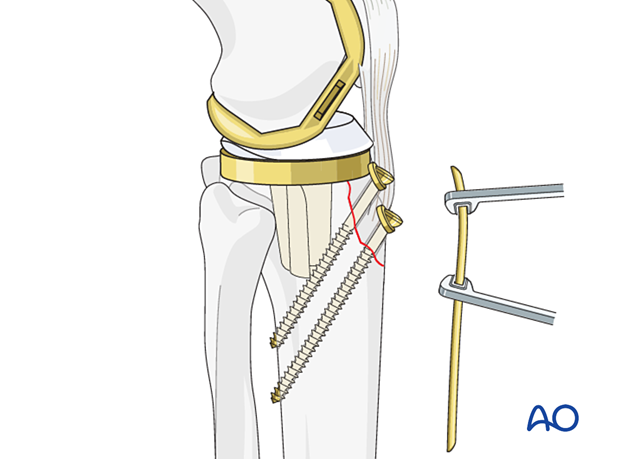
Plate fixation
The plate is fixed to the bone using a mixture of cortical, locking, and non-locking screw fixation.
Options for additional stability
Additional stabilization can be achieved with locking and nonlocking screw fixation above and below the fracture site.
If there is no room for bicortical screw fixation, different options may be used around the component stem to secure the plate:
- Unicortical locking screw fixation
- Cerclage cables integrated into the plate
- Locking attachment plate
For additional details on these implants please refer to adjunct plate options.
Alternative fixation technique
In the setting of a very small or comminuted fragment one or more cerclage constructs or suture anchors can be utilized to reinforce a lag screw or to achieve primary stability. A detailed description of these techniques can be found in the trauma section.
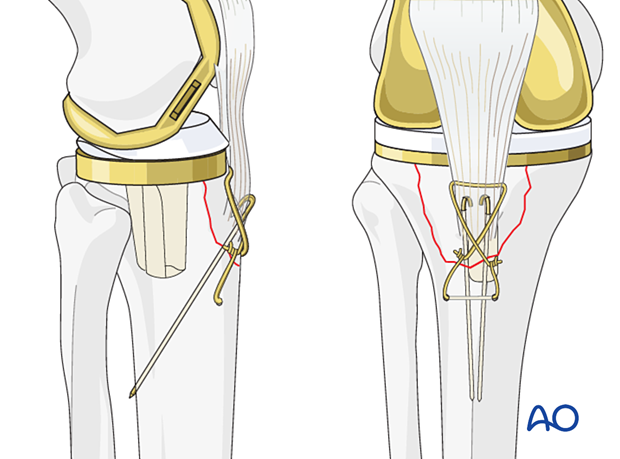
Tubercle fracture repair augmentation
To protect this tubercle fracture repair during the healing process, a protective cerclage wire or suture can be passed around the upper pole of the patella and through a transverse drill hole distal to the tibial tubercle.
This wire frequently breaks later, and it is best to remove it once healing is assured at 3-4 months.
5. Radiographic verification
Anteroposterior, mediolateral, and oblique radiographs of both the fracture site and the arthroplasty are obtained at the end of the procedure, to ensure that:
- There is no displacement
- The joint articulation is preserved
6. Aftercare
The knee is braced in full extension during ambulation for 6 weeks.
Supervised gentle knee flexion can start after wound healing. Resisted knee extension should be limited until 10 weeks or fracture consolidation is visible.












