Patient examination and radiology
1. Visual inspection
Assess the patient for the following signs:
1. Deformity of the elbow and forearm and adjacent joints. Take care to avoid pain during examination.
Extensive swelling in the presence of a proximal forearm fracture may be a sign of elbow dislocation.
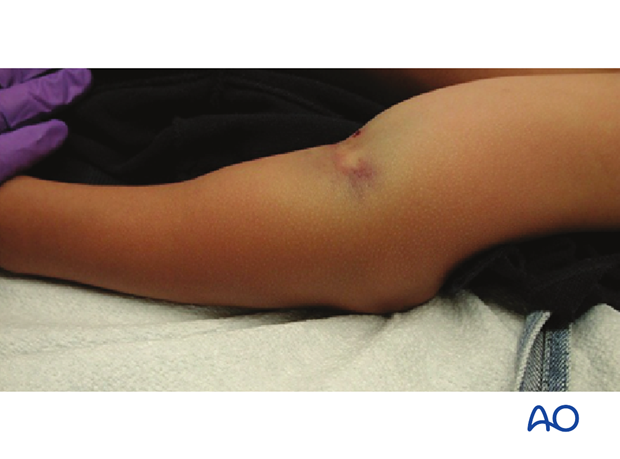
2. Skin discoloration is indicative of severe fracture displacement or of accompanying elbow dislocation.

3. Neurovascular examination:
- Peripheral pulses
- Finger movement
- Cutaneous sensation
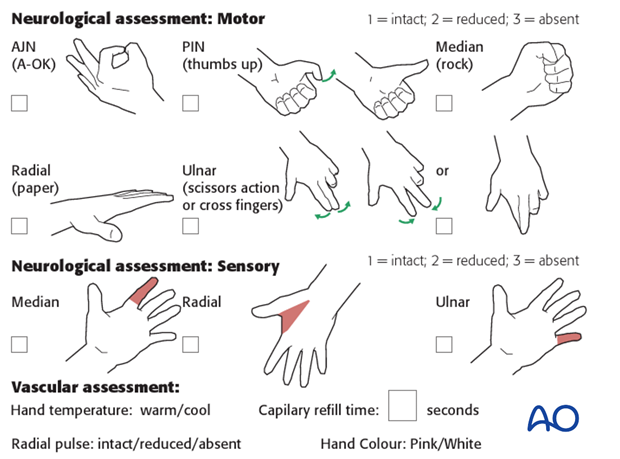
2. Neurological injuries
Neurological injuries in proximal forearm fractures are rare.
Neurological assessment may be difficult and is influenced by the level of pain and the child’s age.
3. Vascular injuries
Vascular injuries in proximal forearm fractures are rare.
The radial pulse is verified by palpation.
The presence of a normal pulse does not exclude compartment syndrome.
4. Preliminary reduction
There is no need for preliminary reduction unless the elbow is dislocated.
Manipulation of a suspected proximal radial fracture may compromise the blood supply to the radial head.
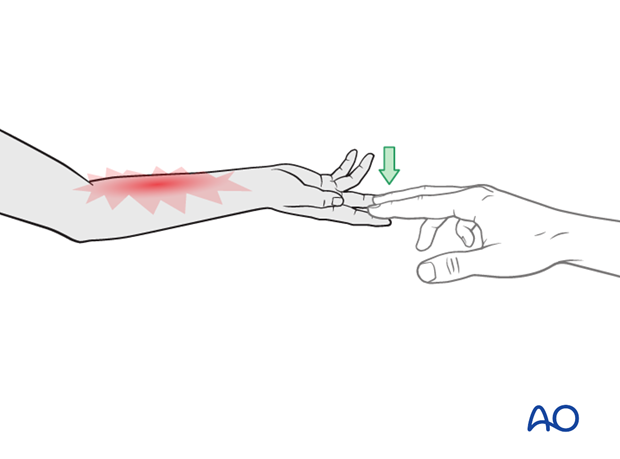
5. Compartment syndrome
Compartment syndrome is an uncommon but devastating complication of upper extremity fractures.
The most straightforward clinical test for evolving muscle ischemia is pain on passive digital extension and/or flexion.
Forearm compartment syndrome and fasciotomy are described in the relevant additional material.
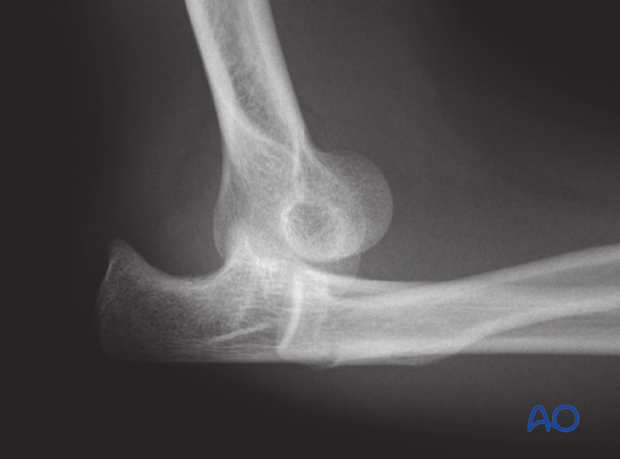
6. X-ray examination of the elbow
The arm is often immobilized in a cast making it difficult to obtain standard x-rays.
Suboptimal x-rays may be sufficient for diagnosis and treatment decisions in proximal forearm fractures.
If the fracture is clearly displaced and surgery is indicated, a further view may be postponed until the patient is under general anesthesia.
Check for associated fractures of the distal humerus (eg, avulsion of medial epicondyle).

7. Commonly overlooked fracture patterns
Check for:
- Combined injuries of radial neck and olecranon
- Avulsion fractures associated with dislocation eg, medial epicondyle or coronoid process












