Compartment syndrome
1. Introduction
Principles
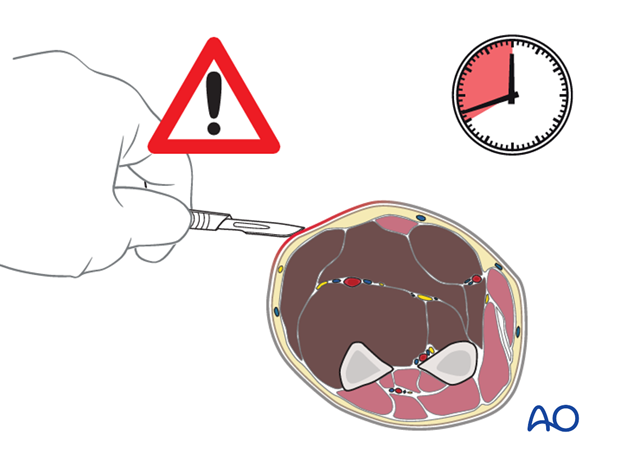
Compartment syndrome is a surgical emergency.
Failure to diagnose it and delays in decompressing the involved compartment(s) can result in major limb disability.
Increasing tissue pressure impedes capillary blood flow and produces vascular stasis and congestion in muscle and nerve tissue. The process is progressive and can lead to ischemic necrosis with permanent loss of function.
Treatment of compartment syndrome requires surgical release of the closed osteo-fascial compartment(s) by extensive division of the skin and fascial envelope.

Incidence
Factures with an ever-present risk of compartment syndrome include:
- Supracondylar humeral fractures
- Segmental fractures
- Displaced forearm shaft fractures
- High-energy distal radius fractures
- Tibial apophyseal avulsions
- Tibial shaft fractures
- High-energy distal tibial fractures
Compartment syndrome may also occur in the thigh, foot and hand.
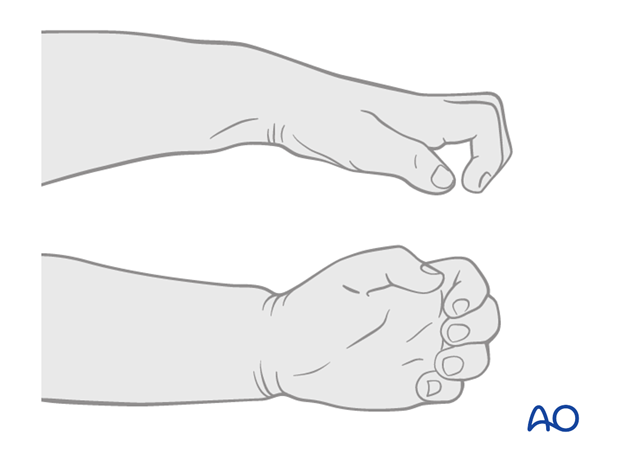
Untreated compartment syndrome results in ischemic necrosis, with loss of nerve and muscle function, as well as joint contracture. This is shown in the illustration of a child with ischemic contraction of the forearm.
Causes
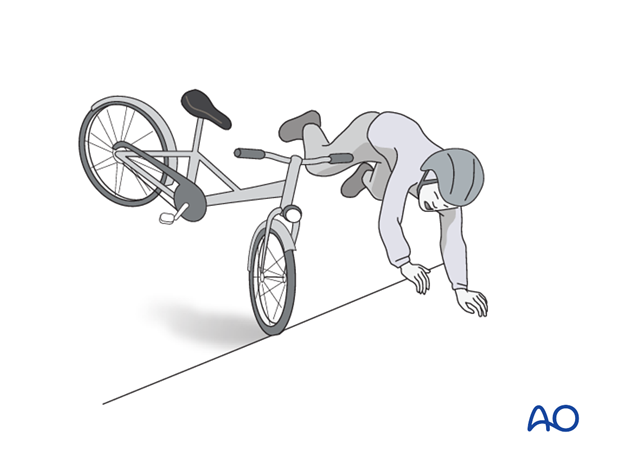
Compartment syndrome occurs most commonly after high-energy limb injuries. However, it can occur after apparently trivial injuries, with or without fractures, or after elective extremity surgery.
Tight bandages, splints, or casts can elevate compartmental pressure and contribute to development of compartment syndrome.
Crushing injuries, burns, or prolonged compression (as may occur in a comatose, unprotected patient), also cause muscle swelling and precipitate the syndrome.
A further cause can be edema from abnormal capillary permeability caused by reperfusion after prolonged ischemia.
Pathophysiology
Compartment syndrome occurs when the tissue pressure within a closed osteo-fascial muscle compartment rises above a level required to maintain blood flow through the capillaries and into the venous drainage system.
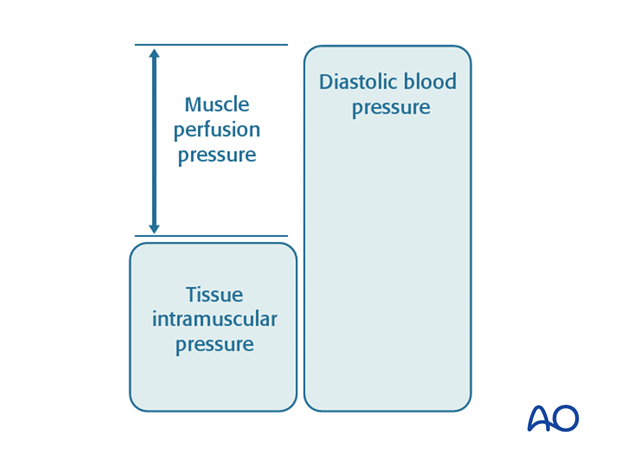
Normal tissue pressure is 0-10 mm Hg. The capillary filling pressure is essentially diastolic arterial pressure. When the tissue pressure approaches the diastolic pressure, capillary blood flow ceases. A number of adult studies have shown that if tissue pressure rises to within 30 mm Hg of diastolic arterial pressure, compartmental capillary blood flow is significantly obstructed and severe hypoxia occurs in muscle and nerve tissue. There are no similar published studies in children.
The critical measurement is muscle perfusion pressure (MPP), the difference between diastolic blood pressure (dBP) and measured intramuscular tissue pressure. (MPP has also represented as ΔP, to indicate the difference between diastolic blood pressure and intramuscular pressure.) This difference in pressure reflects tissue perfusion far more reliably than the absolute intramuscular pressure.
Muscles tolerate short periods of hypoxia, but after a few hours, progressive necrosis begins.
An arterial injury may cause compartmental tissue ischemia. After blood flow is restored, capillaries leak and ischemic muscle swells. Such reperfusion injury is another cause of compartment syndrome.
2. Diagnosis
Symptoms
The diagnosis of this severe complication rests on two factors: a high index of suspicion and a thorough understanding of its variable clinical presentation.
In a conscious and alert patient, there will be unrelenting, worsening pain, greater than expected for the particular injury, and not related to limb position.
It is particularly difficult to evaluate the degree of pain in younger children. Close serial clinical observation will allow judgment of response to analgesics. Persistent crying, or failure to settle, is a concerning sign.
Note: Prior to discharge from the hospital, parents or caregivers should be taught to return for assessment if the child's pain is increasing.
Commonly there is a relatively pain-free interval, perhaps a few hours, following fracture treatment, before such pain develops.
The level of pain can often be judged by increasing requests for ever-stronger analgesia, or increasing use of patient-controlled analgesia (PCA) systems. Any nerve traversing the involved compartment will become hypoxic, often causing numbness and tingling in the nerve distribution. After some hours, ischemic nerves cease to function and the pain resolves.
Pitfall: In children with a fracture and associated neurological deficit, the pain from developing compartment syndrome may well be masked , or partially masked, by the primary nerve injury.
Signs
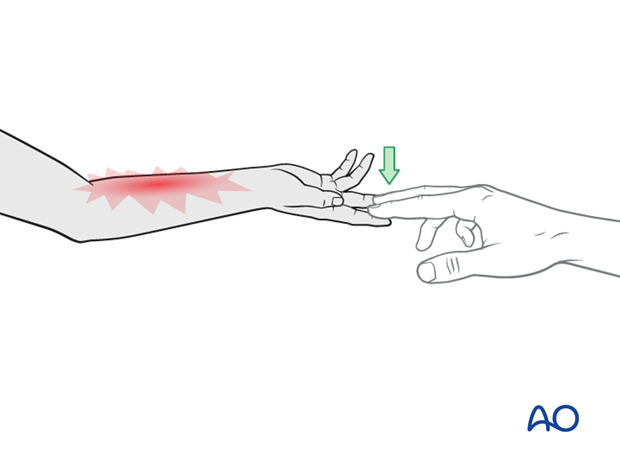
Clinical signs of an impending muscle compartment syndrome include increase in pain on passive muscle stretching.
It is often better to examine children by encouraging active motion that provides passive stretch to the opposite muscle compartments. An increasing arc of active motion is reassuring, but a child with decreasing range of motion and increasing pain is likely to be developing a compartment syndrome.
Tenderness and induration of the affected compartment may be present. Possible sensory (and later motor) deficit in the territory of a nerve traversing the compartment and associated muscle weakness may be noted.
Pitfall: Regional anesthesia can also mask signs and symptoms of compartment syndromes.
The presence of a distal pulse does not exclude compartment syndrome, because in a normotensive patient, the muscle pressure rarely exceeds the systolic level. Measurement of oxygen saturation at the fingertip will not confidently exclude an evolving compartment syndrome.
In an unconscious child, it is easy to overlook a compartment syndrome. Visible limb swelling and unexplained tachycardia are very important nonspecific signs. Direct tissue pressure measurement is helpful for diagnosis in such patients.
Investigation
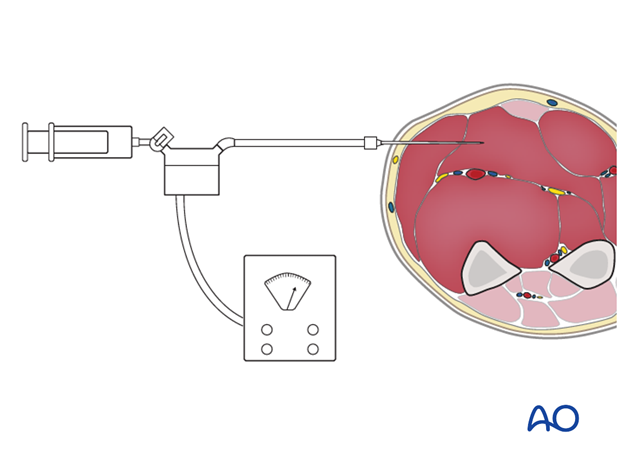
Intracompartmental pressure measurement is a painful procedure and is not well tolerated by most children in the ward setting. It may be used as an adjunctive exam under anesthesia or in an unconscious child in the ICU setting.
When compartment syndrome is clinically obvious, there is usually no benefit from measuring pressures and immediate dermato-fasciotomy should be undertaken.
When the diagnosis is unclear, compartment pressure measurement may be confirmatory, or prevent unnecessary dermato-fasciotomy.
Various techniques are available to measure the intracompartmental tissue pressure.
All trauma surgeons should adopt a technique that is available and familiar. This may involve use of a commercially available compartmental pressure device, a mercury manometer, large-bore needle and connecting tubing (after Whitesides), or an electronic strain gauge used for physiologic monitoring in ICU, or the OR.
In the absence of quantitative evidence of the normal muscle perfusion pressure in children, the comparison between the involved compartment and the corresponding pressure in the uninvolved compartment, in combination with whatever clinical information is available, can inform the surgeon who is responsible for making the decision whether or not to perform a dermato-fasciotomy.
The consequence for the child for failing to perform a dermato-fasciotomy in the presence of a compartment syndrome is a gross functional deficit.
The consequence for the child of performing a dermato-fasciotomy, which subsequently proved to be unnecessary, is a surgical scar. This observation must also inform the decision making.
If the necessary equipment is not available for direct pressure measurement, then the diagnosis must be assumed if there is reasonable clinical suspicion.
Timing
In established compartment syndrome, hypoxic muscle will become necrotic within hours. It is generally accepted in adults that after 6-8 hours of inadequate muscle perfusion pressure (MPP), extensive muscle necrosis is likely and effective release of the muscle compartments involved is unlikely to avoid severe muscle contracture. Similarly, any peripheral nerve passing through the compartment is likely to suffer permanent functional impairment.
There is no hard evidence whether the figure of 6-8 hours can be extended in children.
It is still of paramount importance that the compartment hypertension be released as an emergency intervention.

3. Treatment
If diagnosed within 8 hours
The only appropriate treatment is dermato-fasciotomy of all involved compartments.
Late diagnosis
Where recognition of an established compartment syndrome is delayed for more than 8-10 hours after probable onset, the decision to perform a dermato-fasciotomy requires judgment by the most experienced surgeon available.
This situation is common after mass disasters (eg, earthquakes).
Exposure of partially necrotic muscle has a high risk of wound infection in adults. The benefits of decompressing a compartment with necrotic muscle may be limited. Children have a greater capacity to retain viable muscle for longer.
4. Volar compartment fasciotomy of the forearm
Once a diagnosis of compartment syndrome has been established, or even strongly suspected, each of the relevant compartments must be decompressed fully by extensive dermato-fasciotomy, as a matter of urgency.
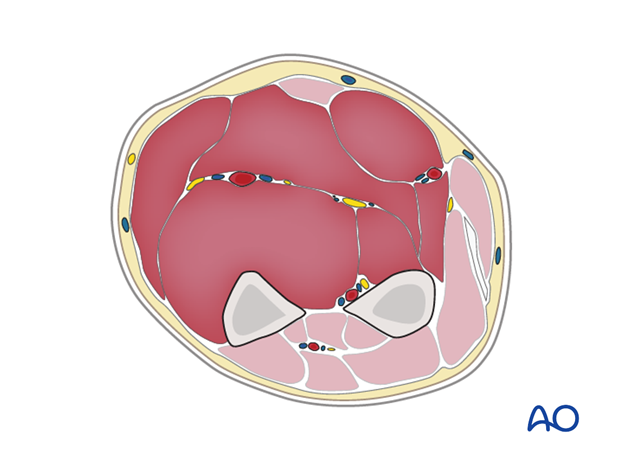
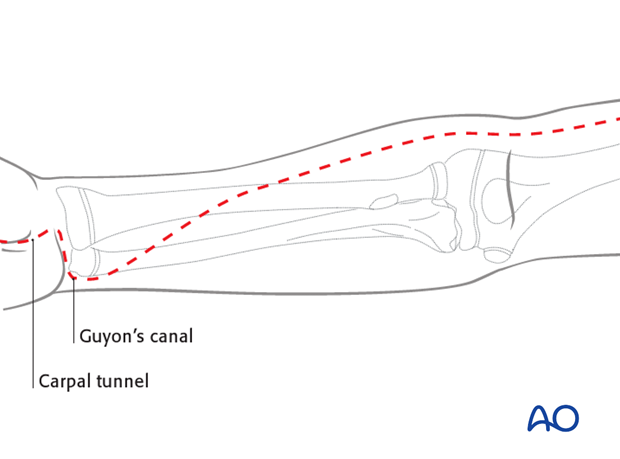
Be aware that there are three main compartments in the forearm (mobile wad, anterior compartment, and dorsal compartment – with each of the latter two being divided into a superficial and a deep portion). The approach to the relevant muscle compartment will be based on one of the standard surgical approaches in the forearm, respecting the important neurovascular structures. The procedure should include decompression of the median nerve in the carpal tunnel and the ulnar nerve in the distal forearm.
The anterior dermato-fasciotomy incision extends over the carpal tunnel and Guyon's canal distally (to decompress the median and ulnar nerves).
It continues with a curved incision towards the radial side of the mid-forearm and proximally on the anterolateral aspect of the forearm, as in a standard Henry approach.
If needed, the dermato-fasciotomy should cross the anterolateral aspect of the elbow, maintaining coverage of the neurovascular bundle running through the cubital fossa in those cases where the wound is left open.
A straight incision across the anterior elbow may result in contracture of the joint.
In the mid-forearm, the curved incision with its apex on the anterolateral aspect of the mid-forearm will expose the flexor compartment.
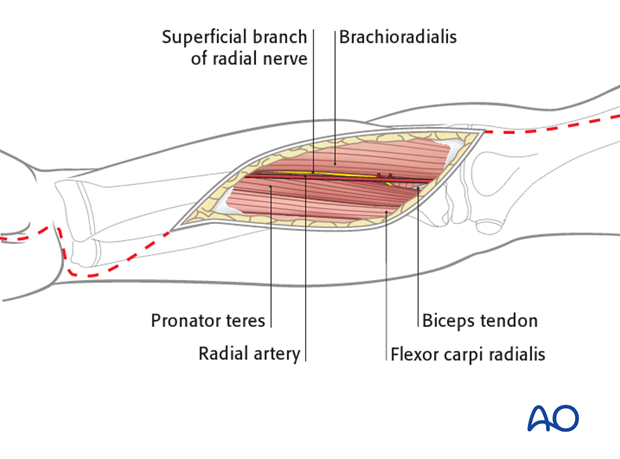
Through this part of the incision, the deep volar compartment may be approached between the radial artery and the flexor carpi radialis muscle.
The artery is retracted laterally (and not medially as with the standard approach to the midshaft of the radius.
The superficial flexor muscle mass is exposed and the overlying fascia released.
This includes the finger and wrist flexors, and exposes the median nerve, which should be identified between the deep and superficial flexor muscles and protected, gently retracting it medially with the superficial flexor muscle mass.
The radial artery is retracted laterally with the brachioradialis muscle and superficial radial nerve, to expose and permit division of the fascia over the deep flexor muscles.
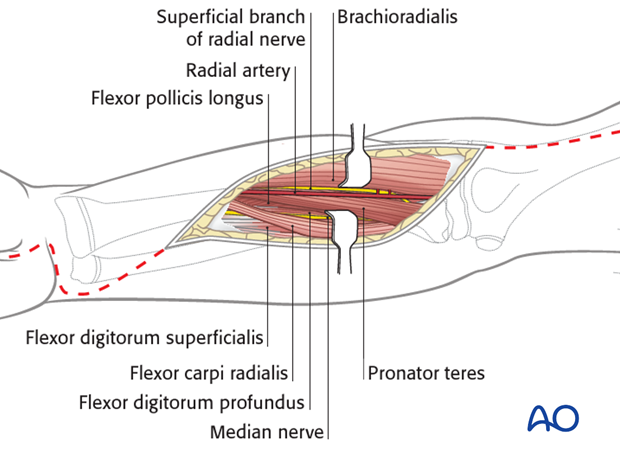
Take note of the path of the median nerve and its cutaneous branch, which runs along the ulnar side of the flexor carpi radialis tendon.
Complete dermato-fasciotomy, including the carpal tunnel, results in extensive exposure and necessitates delayed soft-tissue cover, after reduction of swelling.
This may involve a variety of soft-tissue coverage techniques ranging from progressive delayed closure, using elastic techniques, vacuum closure, to split skin grafting.
See aftercare section.

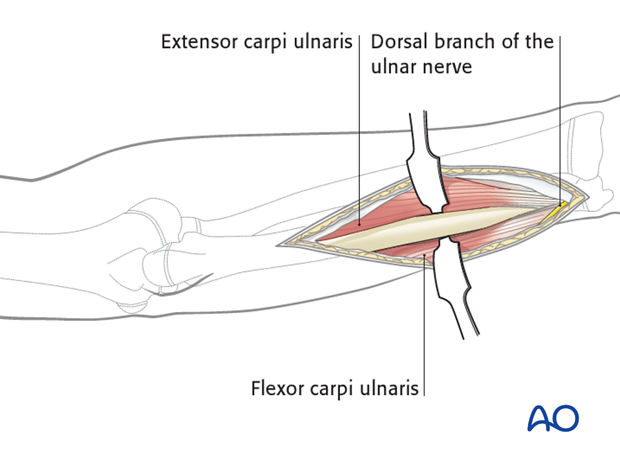
Posterior fasciotomy
An additional approach to the extensor compartment may be necessary.
Note: In the child, full flexor compartment release will usually be sufficient . It is uncommon that a separate posterior fasciotomy is necessary.
Posterior fasciotomy requires a separate posterior approach to the ulna.
Releasing the extensor carpi ulnaris muscle belly from the posterior aspect of the ulna may be sufficient, although there are no data to support this and a clinical decision has to be made during the procedure.
5. Aftercare
Postoperative splintage
It is important to splint the limb in a neutral, or functional position, particularly if muscle damage has occurred, as this predisposes to joint contractures.
Delayed surgical closure
Provided the fasciotomy wound(s) is (are) healthy, the skeletal injury is under control, and the swelling of the soft tissues has sufficiently regressed, consideration must be given to achieving skin coverage.
Split skin grafting is a safe and straightforward technique to cover the healthy soft-tissue defect.
The grafted area can be excised and secondary skin closure performed without tension, when the limb contours have recovered.
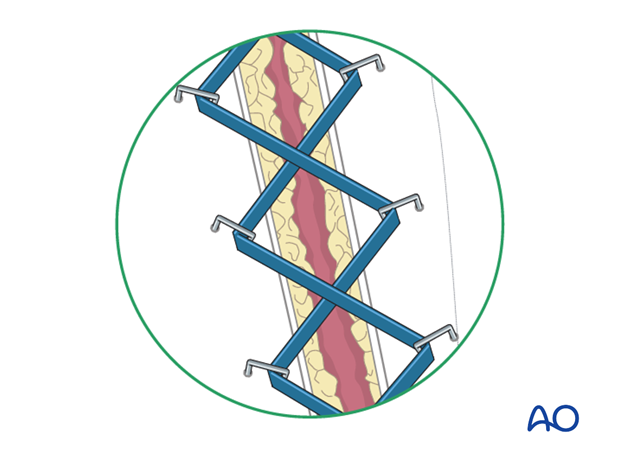
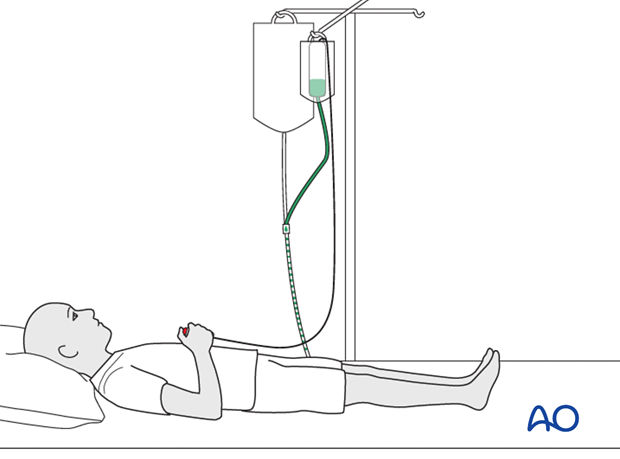
An elastic vessel loop, woven through skin staples, can be tightened progressively as swelling resolves. This can help to reduce the size of the defect to be covered. Care should be taken not to overtighten these elastic bands, which might re-create the compartment syndrome.
Vacuum wound management devices are often used in this setting and they may reduce the swelling more quickly and potentially allow earlier skin closure with less need for grafting.
In many cases, a complete delayed primary closure of a dermato-fasciotomy wound can be achieved in the pediatric patient.