Pediatric polytrauma
1. Introduction
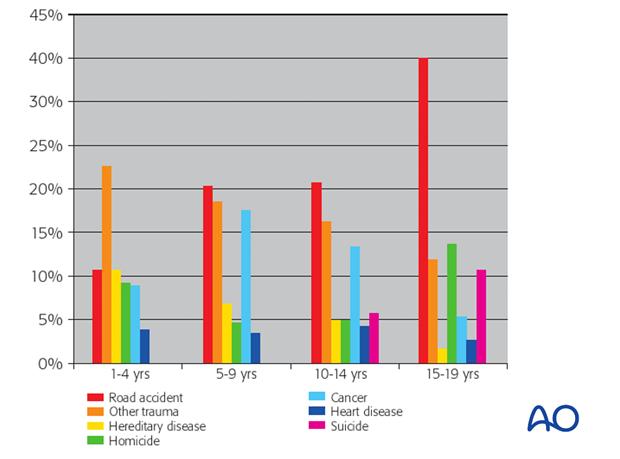
Pediatric trauma is the greatest single cause of death (50%) in children, exceeding all other pathologies combined. [1]
Because approximately 60% of paediatric polytrauma patients suffer fractures of the appendicular skeleton, the orthopaedic surgeon plays a critical part in the care of these patients. [2]
Although rarely intrinsically life-threatening, paediatric musculoskeletal injuries can result in long-term morbidity. An understanding of paediatric physiology and the management of organic and extremity injuries, in the setting of multisystem insult, is essential for the delivery of optimal care to the polytraumatized child.
The principles of trauma care remain the same both for children and adults, but the differences in care required for the optimal treatment of the injured child demand special awareness of the anatomy and physiology of the growing child and adolescent. The body of a child is very elastic, and internal injuries can occur without obvious external signs. [3]
Severely injured children have better survival rates if treated in a specialised paediatric trauma setting. [4]
A total of 53,702 children were analysed, with an overall mortality of 3.9%. The adjusted odds of mortality were 20% lower for children seen at paediatric qualified trauma centres (odds ratio, .80; 95% confidence interval, 68–94). Children aged 3 to 12 years, those with injury severity scores >25 and those with GCS scores <8 all had significant reductions in the likelihood of death at paediatric qualified trauma centres.
2. Emergency assessment
Initial assessment and stabilisation of the paediatric trauma patient in the emergency department is vital. In a study of data in the US National Trauma Data Bank, involving over 220,000 paediatric patients listed therein, defined a number of predictive factors for death in hospital after arrival in the emergency department [5]. These factors included:
- delay between injury and admission
- age
- gender
- ethnicity
- initial vital signs in the emergency department (systolic blood pressure, respiratory rate, body temperature, airway status)
- GCS at the accident locus and in the emergency department
- injury energy
They reported that the risk of death in hospital correlated closely with a GCS score of 3 and a systolic blood pressure <98 mm mercury in the emergency department.
The care of the paediatric polytrauma patient follows the principles of Paediatric Advanced Trauma Life Support which includes rapid diagnosis of respiratory, or circulatory, compromise and correcting problems with oxygenation, ventilation and/or perfusion, in order to prevent cardiorespiratory collapse.
Use of the Broselow Paediatric Emergency Tape and colour-coded equipment trolley is standard for determining height, weight, correct drug doses and drip concentrations in a child, and the appropriate size for resuscitative. [6]

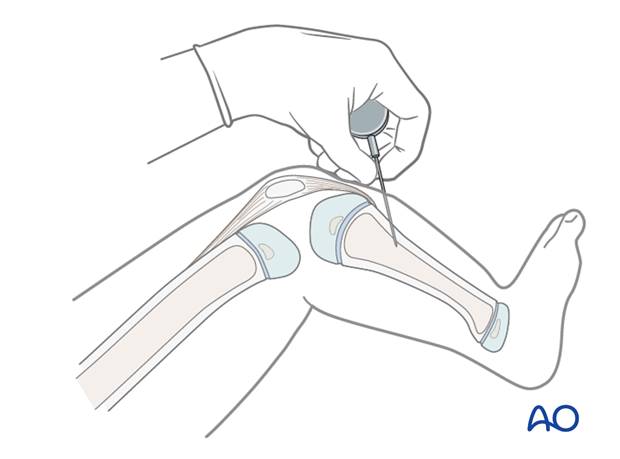
The underlying objective of the primary resuscitative effort is to avoid acidosis, hypothermia and coagulopathy. Perfusion maintenance is critical and large-bore IV access is essential. In cases of difficulty of IV access, intraosseous infusion, via a cannula inserted into the proximal tibial metaphysis, can be used.
The paediatric trauma patient becomes hypotensive when about 25% of the circulating blood volume is lost: delay until this point is reached is highly undesirable and, for this reason, constant monitoring of the heart rate is vital.
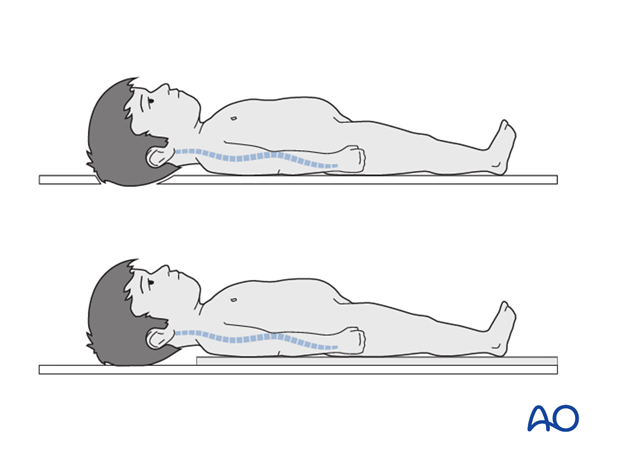
In any child with high energy-transfer injuries, the cervical spine should be stabilised whenever there is suspicion of neck. Pandya et al [7, 8] have emphasised that “children have a relatively larger head in proportion to the rest of the body and a smaller chest size than adults; thus the child’s neck is flexed in an unsafe position when a standard trauma backboard is used. Proper immobilization of the pediatric cervical spine can be achieved by using a backboard with an occipital recess or a mattress pad to elevate the child’s body”
3. Imaging
Initial radiological screening includes AP films of the chest and pelvis, and lateral views of the cervical spine. CT scans of the chest, pelvis and abdomen offer quick diagnostic screening for multisystem visceral injury in the haemodynamically stable child [9].
Secondarily, radiographs of the spine and extremities will follow detailed clinical examination, as dictated by the findings.
4. Splintage
The injured extremities should be splinted. Paediatric patients with femoral and/or unstable pelvic fractures, whose physiological status and other injuries prevent definitive management, can be treated initially with longitudinal skin traction during the initial 24 hours, and thereafter, as necessary, converted to external fixation until definitive care can be undertaken. A pelvic binder may also be used.
5. Physiological response
The physiological responses to major trauma in the child differ from those in the adult.
In adult trauma patients, injury to organ systems leads to a cascade of inflammatory activation, resulting in endothelial permeability, interstitial oedema, intravascular occlusion, microvascular ischemia and eventual multiple organ failure. The rate and overall pattern of multiple organ failure is different in children compared with adults, because of differences in physiology.
Timing of multiple organ failure in paediatric trauma patients differs from that in adult trauma patients. In children, multiple organ failure often occurs early after admission during resuscitation and affects all organs almost simultaneously, whereas organ fail- ure in adults begins 48 hours after injury and occurs sequentially, starting with the lungs. [10-13]
Paediatric versus adult response to multiple injury (after Pandya NK et al, 2013)
| Parameter | Children | Adults |
|---|---|---|
|
Timing of organ failure |
Soon after injury |
>2 days after injury |
|
Organ failure evolution |
Simultaneous |
Sequential |
|
Acute lung injury risk |
Low |
High |
|
Systemic inflammatory reaction |
Muted |
Strong |
|
Local inflammatory reaction |
Strong |
Muted |
|
Morbidity |
Associated with organ damage |
Associated with displaced pelvic fracture |
|
Mortality risk pelvic fracture |
Low |
High |
|
Neurological compromise |
High recovery rate |
Low recovery rate |
Whereas in adults, the fracture fixation philosophy has moved more to “damage control orthopedics” and away from total immediate surgical care, there are few studies on the optimal timing of fracture fixation in children. [15] Valid studies are needed in this field to facilitate evidence-based decision-making about the timing of fracture stabilization and definitive osteosynthesis in polytraumatized children.
6. Osteosynthesis
In the paediatric patient, if the need for osteosynthesis is urgent, it can be undertaken in the early stages of multisystem compromise. As indicated previously, organ failure in children develops soon after injury and tends to resolves quickly after skilled resuscitation and management.
In the polytraumatized child, the individual techniques of osteosynthesis do not differ from those used for isolated skeletal injuries: these techniques are considered in detail in the regional anatomical modules of Pediatric AO Surgery Reference.
7. References
[1] Krug SE, Tuggle DW. Management of pediatric trauma . Pediatrics 2008 Apr;121(4):849-54.
[2] Loder RT. Pediatric polytrauma: Orthopaedic care and hospital course. J Orthop Trauma 1987 Jan;1(1):48-54.
[3] Laurer H , Wurtzler S, Wyen H et al. Quality of prehospital and early clinical care of pediatric trauma patients of school age compared to an adult cohort. A matched-pair analysis of 624 patients from the DGU trauma registry. Unfallchirurg 2009 Sept;112(9):771-777
[4] Oyetunji TA, Haider AH, Downing SR, et al. Treatment outcomes of injured children at adult level 1 trauma centers: Are there benefits from added specialized care? Am J Surg. 2011 Apr;201(4):445-449.
[5] Courville XF, Koval KJ, Carney BT et al. Early prediction of posttraumatic in-hospital mortality in pediatric patients. J Pediatr Orthop 2009 Jul-Aug;29(5):439-444
[6] Luten R, Wears RL, Broselow J et al. Managing the unique size-related issues of pediatric resuscitation: reducing cognitive load with resuscitation aids. Academic Emergency Medicine 2002 Aug;9(8):840-847.
[7] Pandya NK, Upasani VV, Kulkarni VA. The pediatric polytrauma patient: Current concepts. J Am Acad Orthop Surg 2013 Mar;21(3):170-179.
[8] Copley LA, Dormans JP. Cervical spine disorders in infants and children. J Am Acad Orthop Surg 1998 Jul-Aug;6(4):204-214.
[9] Kanz KG, Körner M, Linsenmaier U et al. Priority-oriented shock trauma room management with the integration of multiple-view spiral computed tomography. Unfallchirurg 2004 Oct;107(10):937-944.
[10] Calkins CM , Bensard DD, Moore EE, et al. The injured child is resistant to multiple organ failure: A different inflammatory response? J Trauma 2002 Dec;53(6):1058-1063.
[11] Proulx F, Gauthier M, Nadeau D et al. Timing and predictors of death in pediatric patients with multiple organ system failure. Crit Care Med 1994 Jun;22(6):1025-1031.
[12] Crump JM, Duncan DA, Wears R. Analysis of multiple organ system failure in trauma and nontrauma patients. Am Surg 1988 Dec;54(12):702-708.
[13] Tantaleán JA, León RJ, Santos AA, et al. Multiple organ dysfunction syndrome in children. Pediatr Crit Care Med 2003 Apr;4(2):181-185.
[14] Wood JH, Partrick DA, Johnston RB Jr. The inflammatory response to injury in children. Curr Opin Pediatr 2010 Jun;22(3):315-320
[15] Nahm NJ, Como JJ, Wilber JH, et al. Early appropriate care: Definitive stabilization of femoral fractures within 24 hours of injury is safe in most patients with multiple injuries. J Trauma 2011 Jul;71(1):175-185
Additional reading
- Jakob H, Lustenberger T, Schneidmüller D, et al. Pediatric Polytrauma Management. Eur J Trauma Emerg Surg 2010 Aug;36(4):325-338.
- Pandya NK, Upasani VV, Kulkarni VA. The pediatric polytrauma patient: Current concepts. J Am Acad Orthop Surg 2013 Mar;21(3):170-179.
- An excellent, detailed resource is available at Harbourview Medical Center’s public domain site entitled “ Acute Assessment & Management of Pediatric Trauma: A 7-Module Course Designed for Providers of Early Care to Injured Children” http://depts.washington.edu/pedtraum/
- Another useful resource is PediatricTraumaCareGuidelines2011.pdf from the University of Kentucky.












