Nonaccidental injuries in children
1. Introduction
More than half the victims of child abuse have fractures. The orthopedic surgeon will often be the first person to identify a potentially abused child.
The safest pathway for the child and the clinician is to follow the local child-abuse protocol in all suspicious cases.

2. Case assessment
Any child is a potential victim of nonaccidental injury.
Risk factors
- Single-parent households, particularly father-only households
- Parental, or carer’s, drug or alcohol abuse
- Parental, or carer,’s mental health problems
- Intra-familial violence, or history of violent offending
- Previous child maltreatment in members of the family
- Known maltreatment of animals by the parent, or carer
- Vulnerable and unsupported parents, or carers
- Pre-existing disability in the child

Household income does not relate to risk.

Medical history
Aspects of the medical history can also constitute pointers to potential child abuse.
- History of failure to thrive
- Previous unusual injury (eg, fractured femur in a child 6 months of age)

- A history of a serious high-risk injury, or unexplained death, in a sibling
- Missed immunizations
- Lack of medical records
The context of the alleged event leading to injury may also indicate risk.
- Who witnessed the event?
- Child abuse is unusual in a group setting. If multiple adults witnessed the event, it is more likely to be accidental, and it is easier to verify the history. If possible, the adult witnesses should be interviewed separately

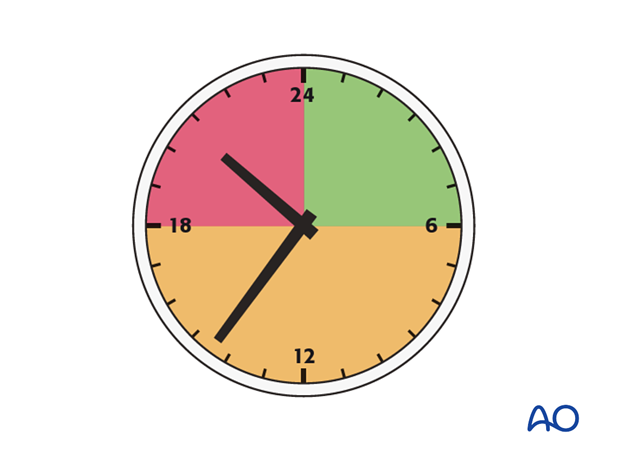
- Was there a delay in seeking medical care? Child abusers tend to delay presenting their injured children
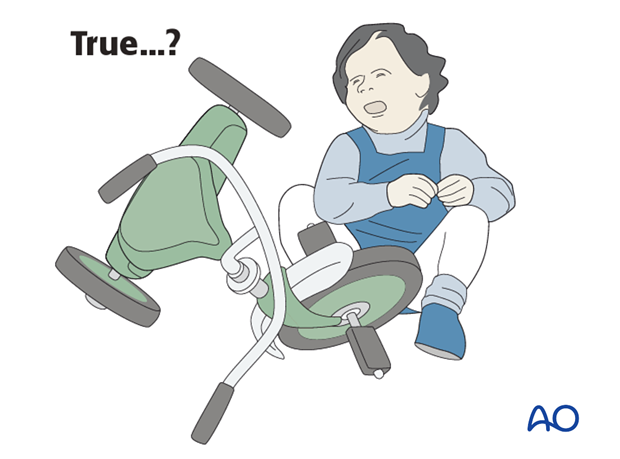
- Is the history plausible?
- What was the mechanism of injury?
- Does the parent's story fit that mechanism?
- Is the history consistent? Parents who have abused their children may modify the medical history over time
Physical examination
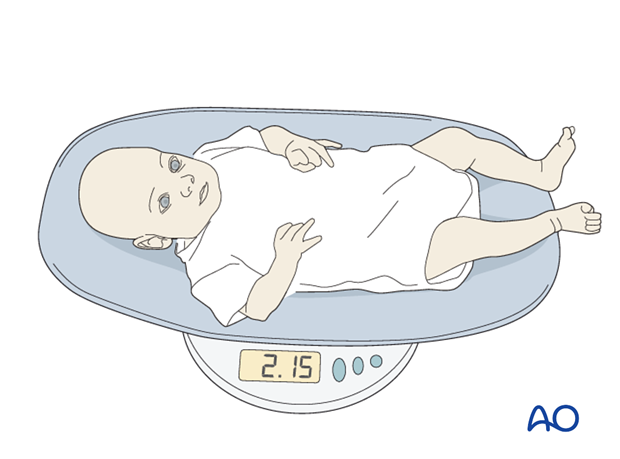
- The child should be weighed and measured, since an abused and/or neglected child is often small for its age
- The classic gaunt, hypervigilant facial appearance of neglect should be recognized

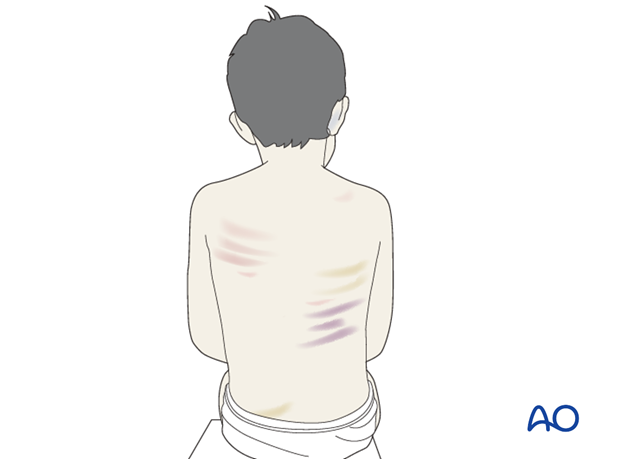
- Every child should be completely undressed and examined for cutaneous injury, including a careful inspection of the genitalia and anus, since many children who are victims of physical abuse may also have been abused sexually

- Facial grip bruising and ear bruising are suspicious
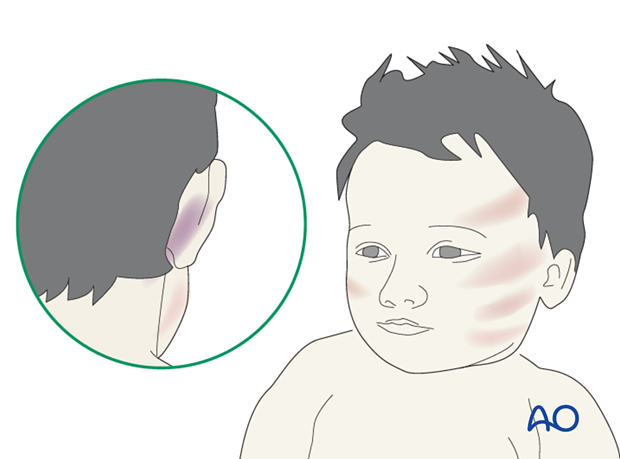
- Bruises of different generations and handprint bruising are also suspicious
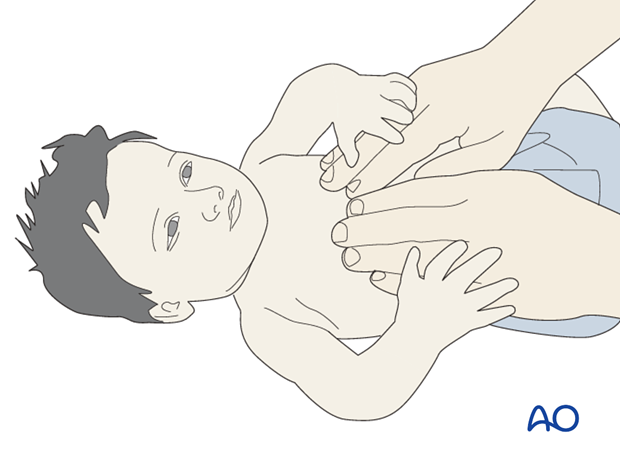
- Palpation over the ribs, the long bones and joints and assessment of joint motion
- Any tender area suggesting a fracture should be x-rayed, even in an older child, in whom a radiological skeletal survey is less valuable
Radiographic indicators
- Spiral fractures of the humerus…

- … or femur, in infants should raise strong suspicions
See: Kemp, A M, Dunstan F, Harrison S, et al. Patterns of skeletal fractures in child abuse: systematic review. BMJ 2008 Oct 2;(337): a1518. This article concluded:
“When infants and toddlers present with a fracture in the absence of a confirmed cause, physical abuse should be considered as a potential cause. No fracture, on its own, can distinguish an abusive from a non-abusive cause. During the assessment of individual fractures, the site, fracture type, and developmental stage of the child can help to determine the likelihood of abuse.

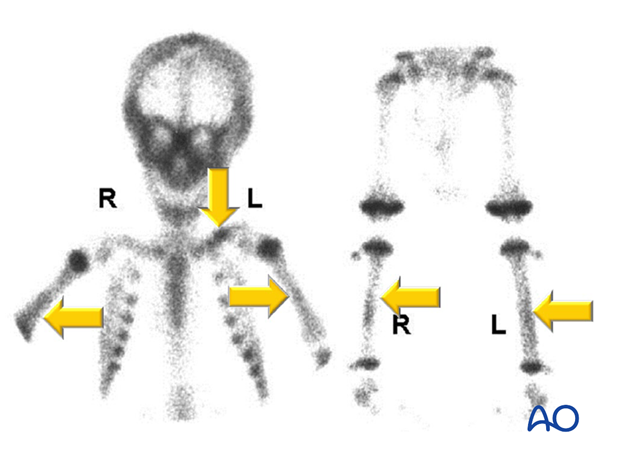
- A dedicated skeletal survey should be obtained in any child less than 2 years of age in whom there is a suspicion of physical abuse
- Multiple rib fractures, especially at different stages of healing are very suspicious

- Limb fractures at different stages of healing are also very suspicious

- In order to exclude intracranial injury, a CT scan of the head should be performed whenever there is a strong suspicion of nonaccidental injury
- Fundoscopy should also be performed to identify retinal hemorrhages
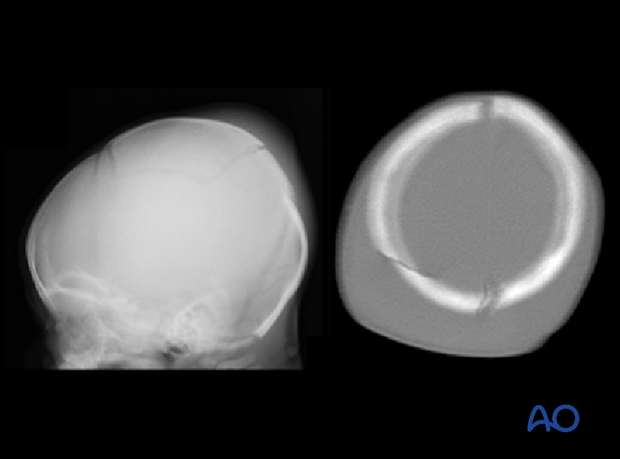
- If the skeletal survey is negative and there is still strong clinical suspicion of fracture, an isotope bone scan may identify fractures and areas of subperiosteal new bone formation, not demonstrated on a single radiological examination. An alternative is repeated radiological examination after an interval of 2-3 weeks
Other studies
Because children with certain genetic syndromes can bruise more easily, if the physical examination suggests a syndrome (eg, laxity of skin and hypermobile joints as seen in Ehlers-Danlos syndrome), a specialized genetic evaluation is indicated.

The most troublesome differential diagnosis is between nonaccidental injuries and osteogenesis imperfecta (OI).
OI is protean in its manifestations and in 1979, Sillence classified five types, based on clinical and radiological features. This classification has since been modified in the light of further genetic data.
See:
- Van Dijk FS, Pals G, Van Rijn RR, et al. Classification of Osteogenesis Imperfecta revisited. Eur J Med Genet. 2010 Jan-Feb;53(1):1-5.
The classical blue sclera are not always present and the onset of fractures can be delayed. It is a difficult diagnosis to substantiate and is the province of specialist pediatricians and geneticists.
If a child presents with unexplained fractures and none of the risk factors for nonaccidental injuries is present, then OI has to be considered by appropriate experts.
In 1995, Roger Smith of Oxford stated “The distinction between NAI and osteogenesis imperfecta is a small and untidy corner of pediatrics. Osteogenesis imperfecta is rare and few people have extensive experience of it; the views of those who have should be taken into account, irrespective of their specialty. Where legally necessary biochemical confirmation of osteogenesis imperfecta should be sought.” ( Smith R. Osteogenesis imperfecta, non-accidental injury, and temporary brittle bone disease. Arch Dis Child. 1995 Feb;72(2):169-176.)
3. Documentation
Document everything through:
- Detailed written records
- Voice recording
- Photography
- Video recording