Complications and technical failures
1. Introduction
Femoral fractures are often high-energy injuries and are associated with significant but predictable complications.
Treatment related complications can be minimized by anticipating them and paying attention to the general principles of fracture management.
2. Delayed union and nonunion
Delayed union and nonunion are rare in femoral shaft fractures due to excellent muscle coverage.
Causes:
- Persistent fracture gap
- Delayed weight bearing
- External fixation
- Open plating
- Infection
- Devascularization
- Bone loss
- Vitamin D deficiency
Prevention:
- Confirm reduction before definitive fixation
- Compress fracture before finalizing fixation
- Start immediate partial weight bearing
- Select biologically appropriate fixation where possible (intramedullary nailing > MIPO > open plating > external fixation)
- Vitamin D supplementation
- Prophylactic antibiotics
- Systematic debridement of open fractures
3. Refracture
Refracture is uncommon with intramedullary fixation.
Factors contributing to delayed union and nonunion also increase the risk of refracture.
Causes:
- Premature removal of external fixator
- Removal of plate
- Malunion
Prevention:
- Partial weight bearing with crutches following implant removal
- Activity modification until sufficient bone strength
4. Malunion
Causes:
- Unequal ESIN sizes
- Unequal ESIN bend
- Inappropriate use of ESIN (> 50 kg)
- Use of external fixator
Prevention:
- Use locked reamed nails for femurs of adequate size
- Attention to detail in ESIN selection and bending
- Avoid use of external fixator, unless no practical alternative
5. Rotational malunion
Causes:
- Difficulty assessing intraoperative rotational alignment
Prevention:
- Use multiple methods to assess rotational alignment after provisional and final fixation (see the additional material on assessment of rotation)
6. Implant pain/prominence
Causes:
- Large plates especially proximally and distally
- Long screws
- Growth and metaphyseal modeling
Prevention:
- Use intramedullary devices
- Measure screw length carefully
- Anticipate prominence of screws and nail ends after metaphyseal growth especially in patients of 9 years and younger
7. Muscle scarring and knee stiffness
Causes:
- Prolonged immobilization
- Pain preventing early motion
- Instability preventing early motion
- Comminution of anterior distal femur
- Extensive soft-tissue injury
Prevention:
- Stable fixation
- Early active motion
- Manipulation of knee through full range after applying an external fixator
- Continuous passive motion in high risk patients
8. Peri-implant fracture
Causes:
- Stress riser from plate or short nail
- Pathological bone (eg, osteogenesis imperfecta)
- Disuse osteopenia
Prevention:
- Intramedullary fixation where possible
- Early partial weight bearing
9. Leg-length discrepancy
Causes:
- Length unstable fracture
- Spiral fracture treated with cast
- Segmental fracture treated with cast
- Spiral fracture treated with ESIN
- Segmental fracture treated with ESIN
Prevention:
- Avoid early weight bearing if fixation is length unstable
- Achieve stable construct
- Consider MIPO
- Consider end caps for ESIN
Consider reevaluation of leg length after one year when most of the effect of overgrowth will be apparent.
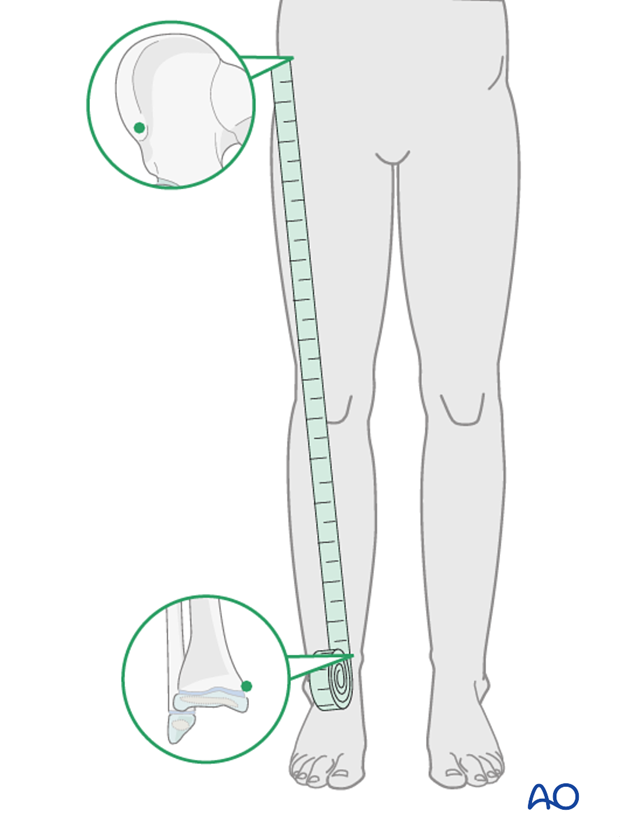
Clinical assessment of leg length uses a tape measure from the ASIS to the medial malleolus.
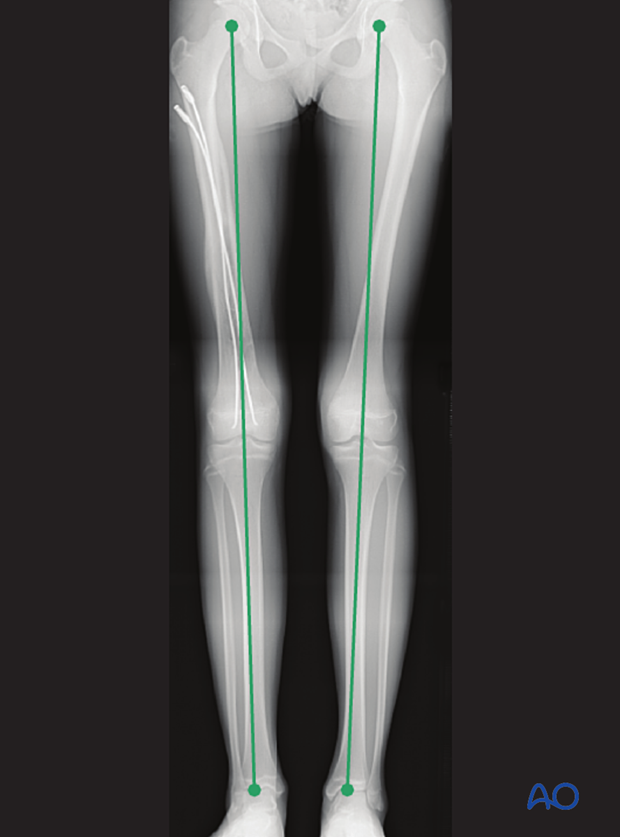
In a long-leg x-ray the leg length is measured between the radiographical landmarks femoral head and ankle joint.
10. Angular deformity
Causes:
- Fracture malunion (see above)
- Occult growth plate injury
- Valgus overgrowth after plating of distal-third fractures
Prevention:
- Achieve adequate fracture reduction and implant stability
- Avoid injury of the distal growth plate with instruments and implants
- Early and repeated assessment of growth or physeal injury after high-energy mechanisms (motor vehicle trauma)
- Early and repeated assessment of growth or physeal injury after plating of distal third fractures












