Minimally invasive osteosynthesis approach to the pediatric femoral shaft
1. Introduction
Approaches for minimally invasive plate osteosynthesis are usually performed laterally. They vary according to the fracture location: proximal, midshaft, or distal.
2. Principles
The advantages of minimally invasive plate osteosynthesis of the femoral shaft include reducing the extent of muscle detachment and limiting the effect on bone vascularity.
Approaches for minimally invasive plate osteosynthesis are usually performed laterally.
A minimum of one small incision to approach the bone is required to place the plate.
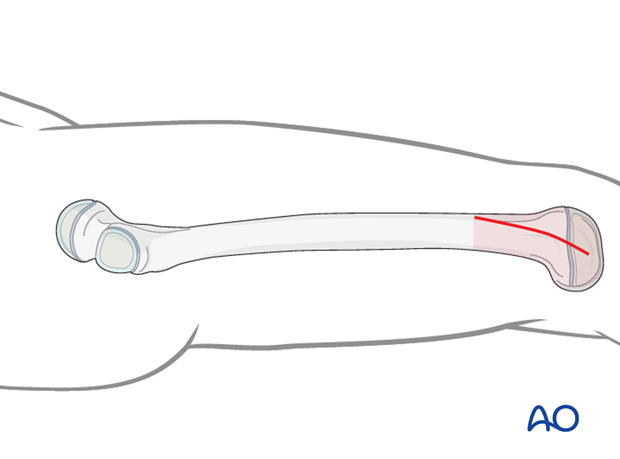
A distal approach is most commonly used for fractures in the distal third of the shaft.
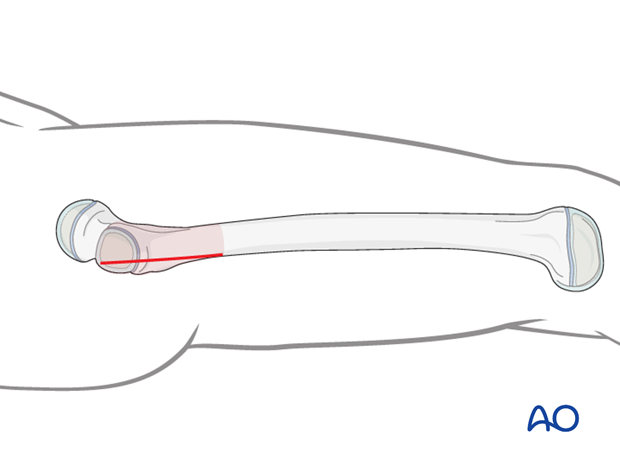
A proximal approach is most commonly used for fractures in the proximal third of the shaft.
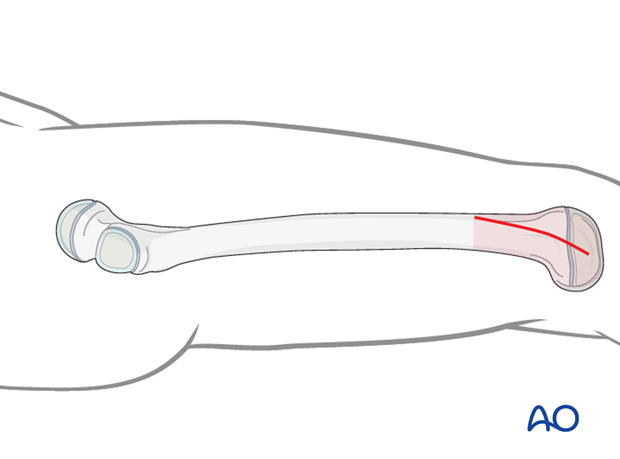
Midshaft fractures can be approached from either end and the position of the incision can be moved towards the fracture providing better access to the diaphysis.
Additional screws can usually be placed through stab incisions. In some cases, a second small approach is required at the fracture site or at the far end of the plate to allow direct manipulation.
Thorough preoperative planning is compulsory to define the location of the most suitable approach.
3. MIO approach to the distal femur
Perform a lateral incision as far as the femoral epicondyle distally.
The starting point and length of the incision can be adapted to suit operational requirements.
Incise the fascia lata and split it along its fibers, parallel to the skin incision.
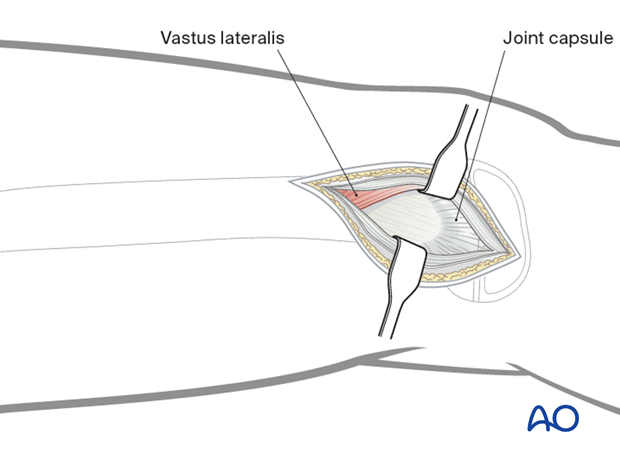
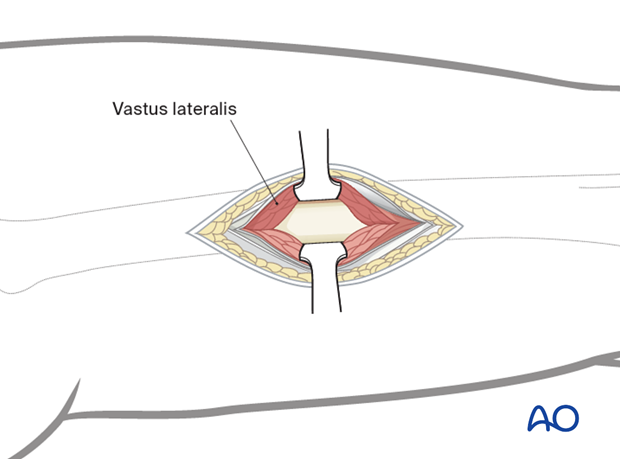
Mobilize the inferior margin of the vastus lateralis and retract the muscle anteriorly. The plane between the femur and vastus lateralis is the entry point for the plate.
Closure
Allow the vastus lateralis to fall back over the plate and femur and close the tensor fascia lata.
The subcutaneous tissue and skin are closed according to surgeon’s preference.
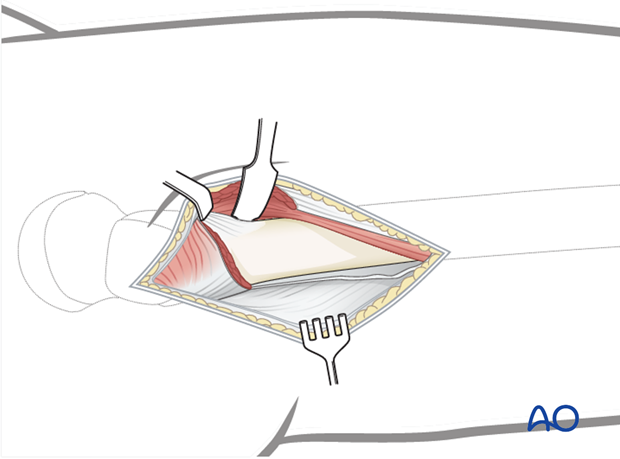
4. MIO approach to the subtrochanteric region
Start the lateral proximal incision at the greater trochanter and continue distally as far as needed.
Incise the fascia lata with a scalpel and split it with scissors, parallel to the skin incision.
Expose the fascia over the vastus lateralis.
If exposure of the proximal femoral shaft is necessary, identify the origin of the vastus lateralis.
Perform an extraperiosteal L-shape incision and retract the muscle anteriorly.
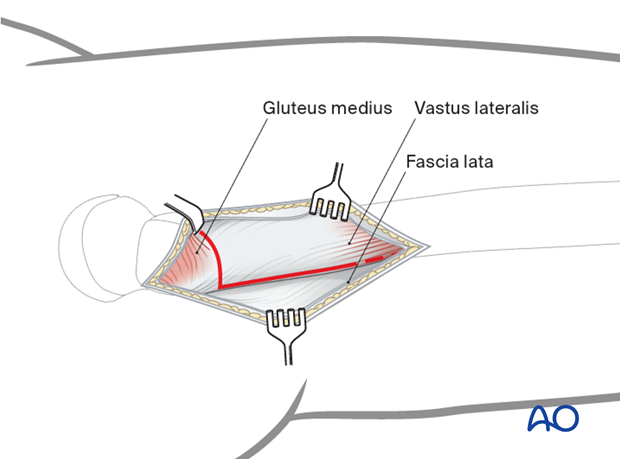
Elevate the vastus lateralis sufficiently to allow submuscular plate insertion.
Closure
Repair the origin of vastus lateralis and close the tensor fascia lata.
The subcutaneous tissue and skin are closed according to surgeon’s preference.
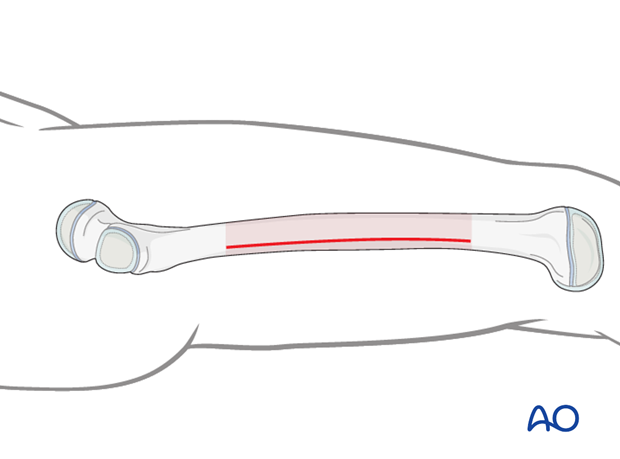
5. MIO approach to the femoral shaft
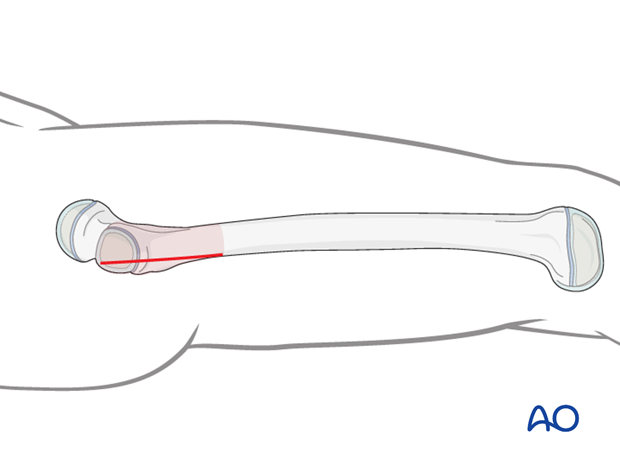
Perform a short incision along a line between the lateral femoral epicondyle and the greater trochanter.
The starting point and the length of the incision depend on the operational requirements for the minimally invasive procedure.
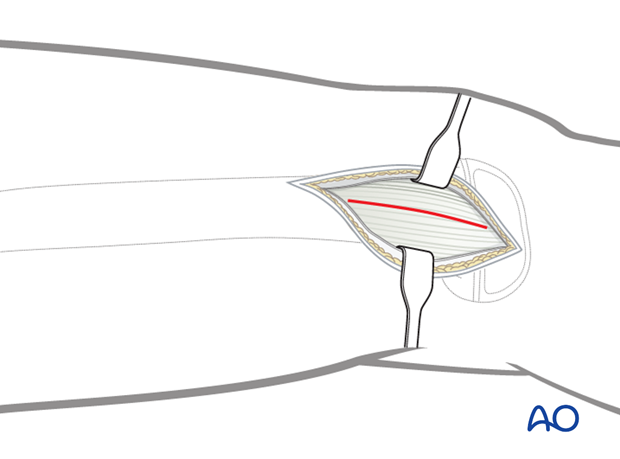
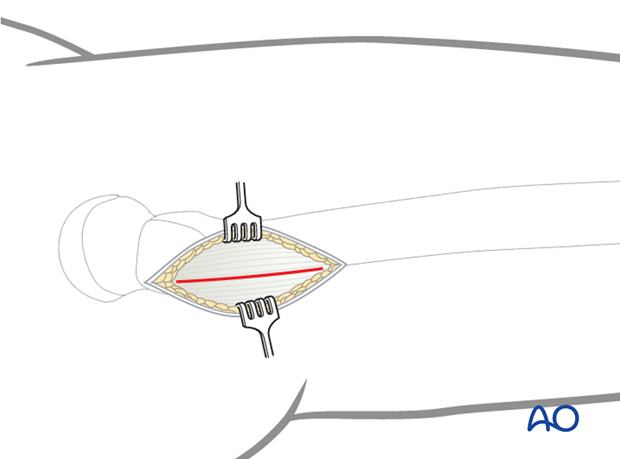
Incise the fascia lata and expose the fascia of the vastus lateralis.
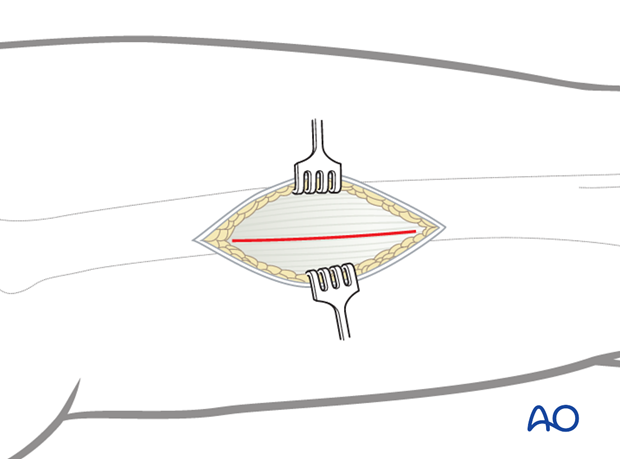
Incise the fascia of the vastus lateralis.
This small lateral incision provides enough access without devascularization of muscle.
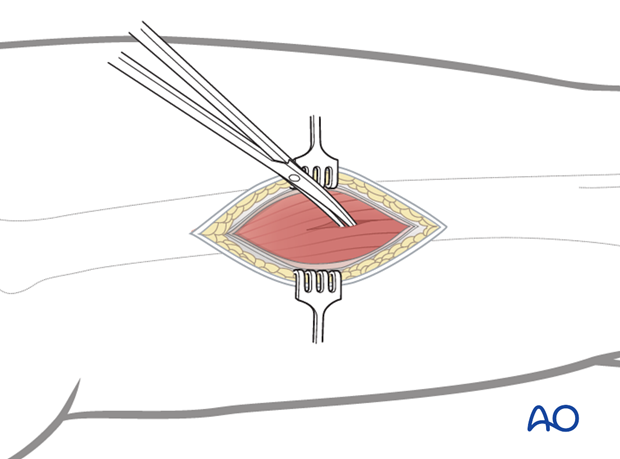
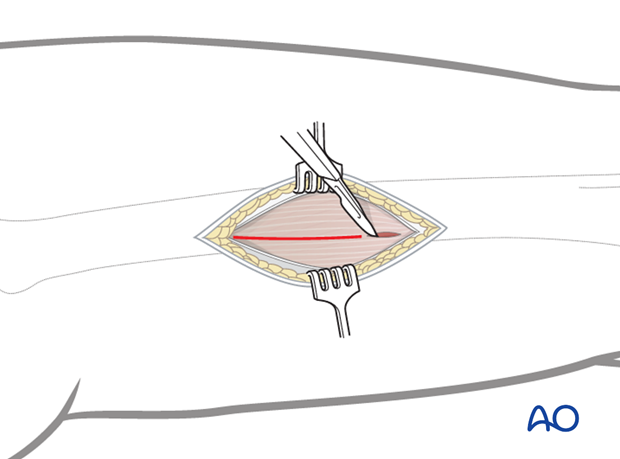
Perform blunt dissection directly through the belly of the vastus lateralis to the bone.
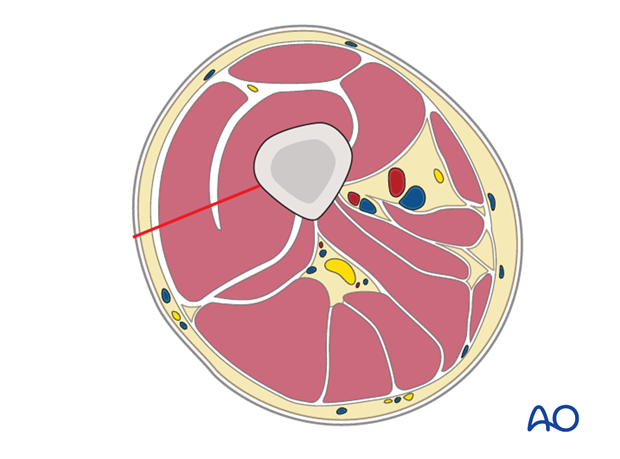
The use of one anterior and one posterior extraperiosteal Hohmann retractors is recommended for exposure of the femoral shaft. These retractors also assist with accurate plate positioning on the femur.
Closure
Allow the vastus lateralis to fall back over the top of the lateral femur and close the tensor fascia lata.
The subcutaneous tissue and skin are closed according to surgeon’s preference.












