Approach to the anterolateral surface of the tibia
1. Indications
The anterolateral approach, through an incision slightly lateral to the tibial crest, reflects the anterior compartment muscles from the lateral tibial surface.
This approach is used uncommonly, but may be necessary when the medial soft tissues are compromised, such as with open fractures, as illustrated, where the wound overlies the site for a medial plate.
The disadvantage of this approach is, that the exposure is more difficult, because the surgeon must mobilize the muscles of the anterior compartment. It also compromises the tibial blood supply.

2. Anatomy
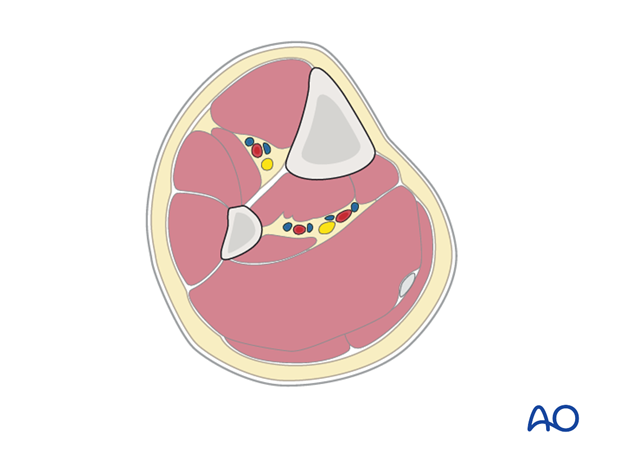
Triangular shape of the tibia
The lateral and posterior surfaces of the tibia are covered by muscle. The anteromedial surface has only a thin layer of subcutaneous tissue and skin. This surface provides less blood supply to the underlying bone.
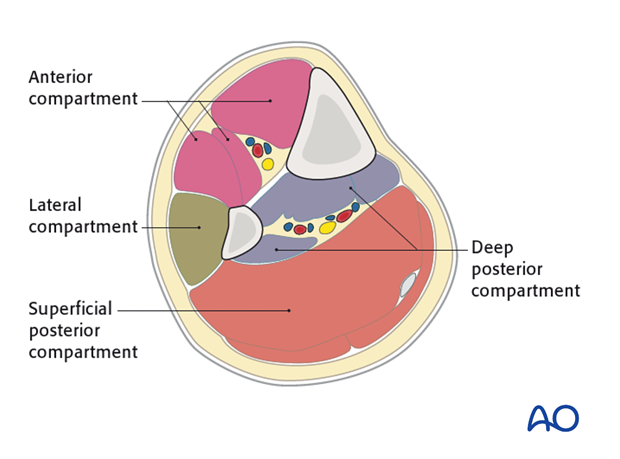
The lower leg has four compartments:
- Anterior
- Lateral
- Deep posterior
- Superficial posterior
The anterior compartment has three muscles and one main artery and nerve: Tibialis anterior, extensor hallucis longus, extensor digitorum longus; the anterior tibial artery and deep peroneal nerve.
The lateral compartment has two muscles and one nerve. The muscles are the peroneus longus and brevis and the superficial peroneal nerve.
The deep posterior compartment has three muscles and two arteries and one nerve: The muscles are the tibialis posterior, the flexor hallucis longus and the flexor digitorum longus. It also has the peroneal artery and the posterior tibial artery as well as the tibial nerve.
The superficial posterior compartment has just two muscles in it: The gastrocnemis and soleus muscles and the sural nerve.
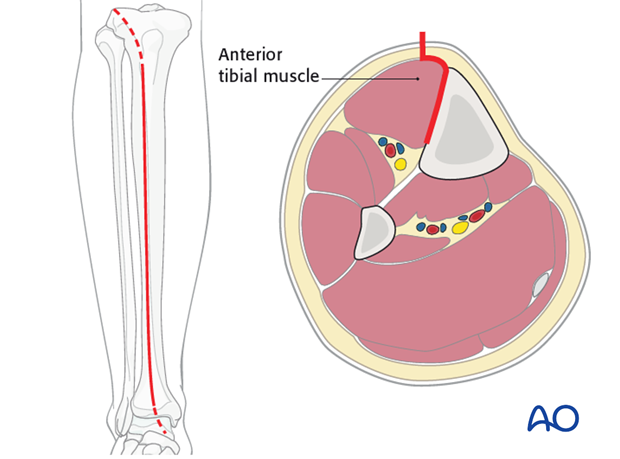
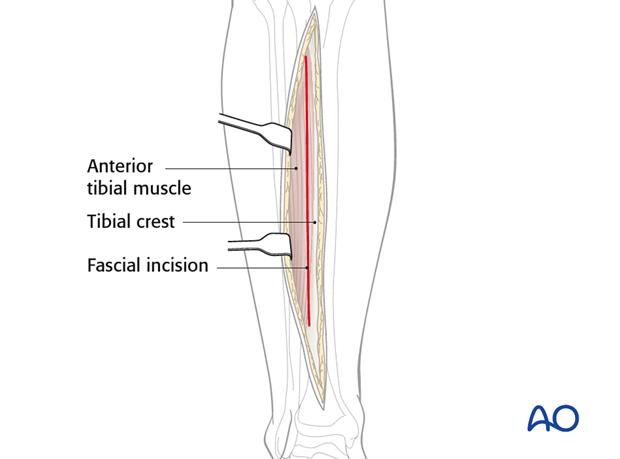
3. Skin incision
A longitudinal incision lies 1-2 cm lateral to the tibial crest and continues distally straight over the ankle joint along the line of the anterior tibial tendon.
The length of the incision depends on the plate length.
The distal extension of the anterolateral approach is helpful for distal tibial fractures, but is obstructed by muscles and neurovascular structures of the anterior compartment.
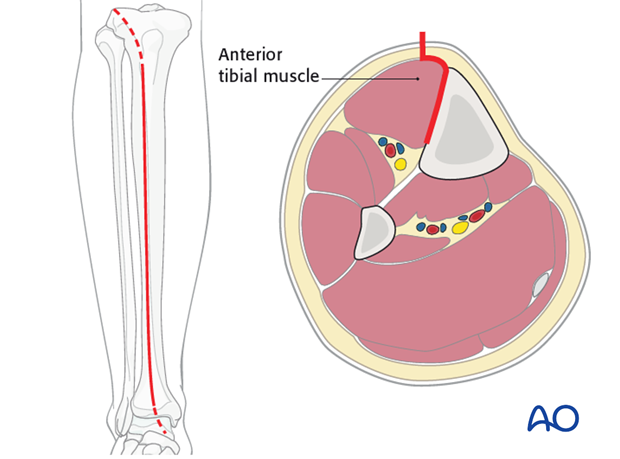
4. Dissection
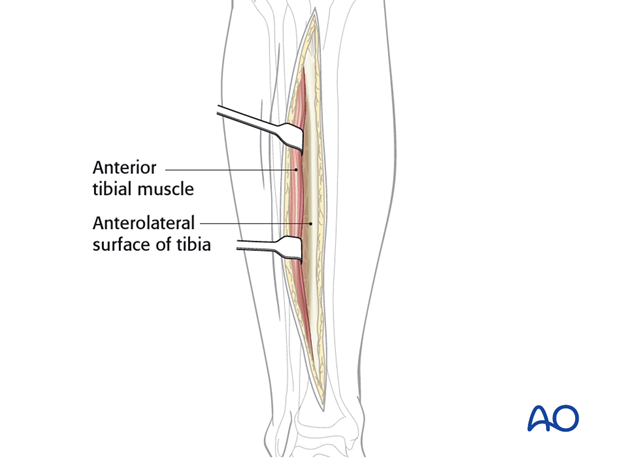
The fascia is incised just lateral to the tibial crest and the dissection is carried down extraperiostally along the lateral surface of the tibia.
The periosteum is left intact, though it may require mobilization near the fracture site for exposure of fracture edges. This is commonly done in preparation for direct anatomical reduction.
Retraction of the tibialis anterior muscle should be limited, to show only the essential part of the anterolateral surface of the tibia.
Near the junction of the middle and lower thirds of the tibia, the anterior compartment vessels (Anterior Tibial) and nerve (Deep Peroneal) come together and approach the lateral tibial surface. They wrap obliquely anteriorly and distally around the tibia. In the distal metaphyseal area, they lie on the periosteum, under the myotendinous portion of tibialis anterior, extensor hallucis longus, and extensor digitorum longus. If this exposure extends into the distal third of the tibia, the surgeon should identify and protect the neurovascular bundle. With care, it can be mobilized from the tibial surface, along with the anterior compartment muscles. This makes it possible to pass a plate more distally on the anterolateral surface, all the way to the ankle joint, if necessary.
5. Wound closure
Only the skin and subcutaneous tissues should be closed. The fascia should be left open. This is important to minimize the risk of compartment syndrome.












