Combined hindfoot injuries
1. Principles
Introduction
Often, these cases present dramatically from high-energy trauma. Subtalar dislocations, open hindfoot injuries and near amputations all may result from complex hindfoot injuries. Treatment is usually emergent and based upon principles of open fracture management. Stepwise care and reconstruction of the soft tissues and hindfoot is a mainstay for success.

Emergency management
Primary emergency management would always include care of the patient as a whole and stabilization of life-threatening injuries before dealing with the significant hindfoot injury. Tetanus prophylaxis, antibiotics and reduction of severe fractures and dislocations with appropriate investigation allows for primary surgical management and secondary definitive care.

Injury
Presentation may be in the form of dislocations, fracture dislocations, or severe open fractures. Principles of treatment follow well-established algorithms for management of the patient, limb and fracture.
In this anatomic region, because of the delicate soft tissues and intricacy of articular surfaces, accurate reduction of injuries and soft-tissue care is mandated.

Unfortunately, severe injury often ends up with marked patient disability and poor functional outcomes. In this anatomic region, there is a spectrum of injuries which may result in good outcomes, or, on the other hand, a bad outcome and an amputation.
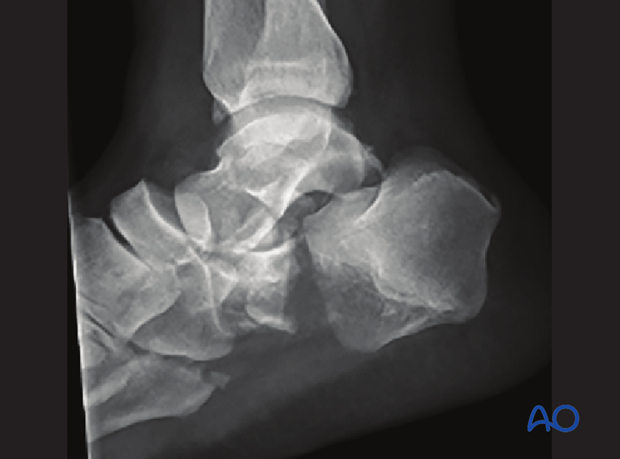
Radiology
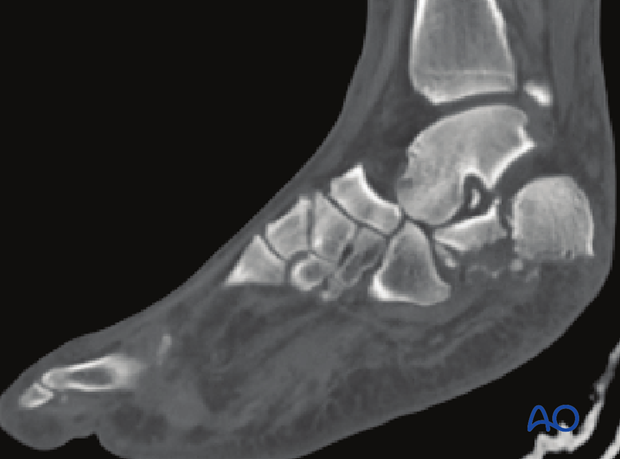
X-ray, CT scans and other imaging is necessary. Complex imaging such as CT scans is best done once the deformities have been corrected and preliminary reduction carried out.
The CT scans are most helpful in demonstrating all the intricacies of the anatomical derangement. It is most helpful first in providing full understanding of the fracture morphology, and then in planning a rationale for reduction and fixation.
2. Primary operative management
External fixation
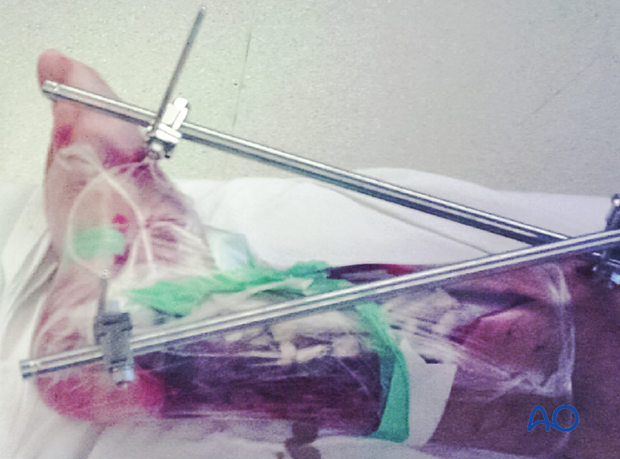
Initial operative treatment consists of irrigation and debridement which is followed by reduction and stabilization. Because of the complexity of the fractures and soft-tissue injuries, external fixation is all that one uses initially. Each case has to be considered on its own merits. However, in each instance one should use the well-proven principles of treatment.
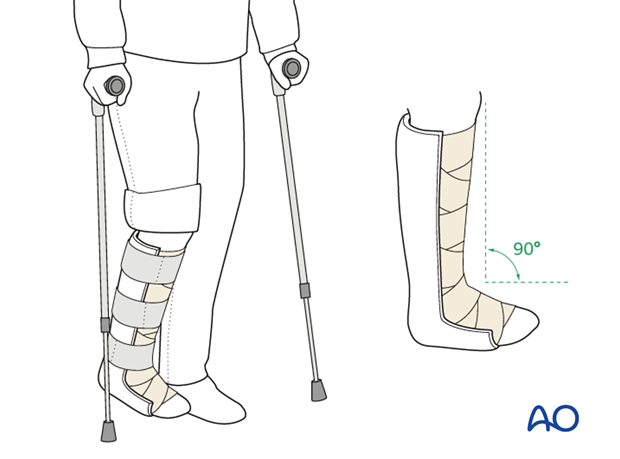
As elsewhere in the body, application of an external fixator after soft-tissue care creates the best environment for initial limb management. The external fixator should be placed outside the zone of injury, with normal anatomy restored. The foot is best positioned at 90 degrees to the limb with pins in the tibia, talus, midfoot, or forefoot, as needed in the particular case.
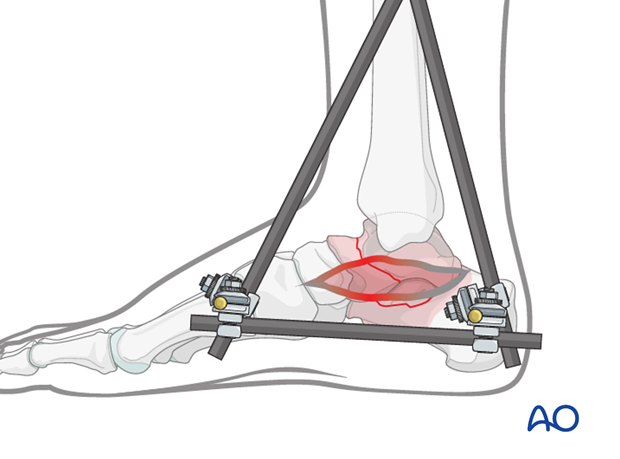
The external fixator provides stability for the bony components of the foot. The soft tissues are put to rest and soft-tissue deficits are identified, should flaps or grafting be needed.
The external fixator is placed by the surgeon using bony anatomy that is stable and spanning areas of instability and soft-tissue loss.
Occasionally, percutaneous pinning is also advisable because of gross instability within the hindfoot and midfoot.
Instability treated by pinning
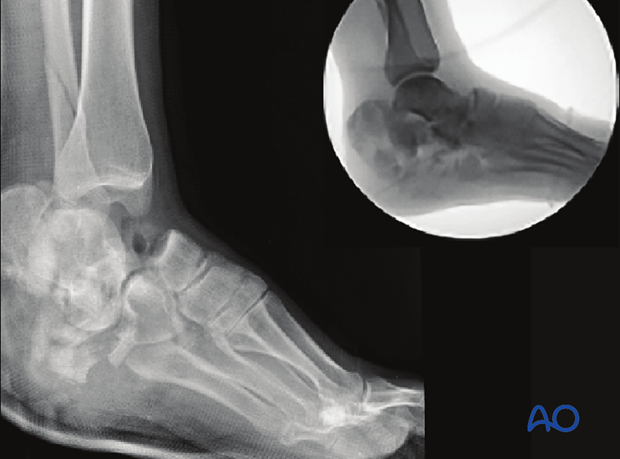
The image shows a closed injury. The calcaneus is broken between the middle and the posterior facets and turned 90 degrees from its normal anatomic position.

This gross instability was reduced and temporarily pinned.
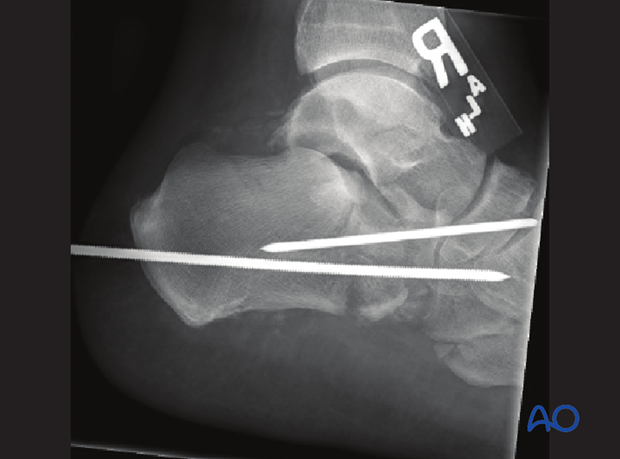
No further definitive operative care was undertaken until the soft tissues settled.

Severe fracture with bone loss and soft-tissue management
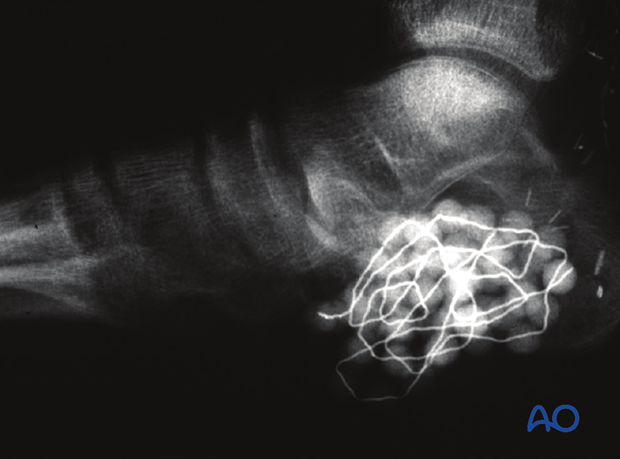
This x-ray image shows an open calcaneal fracture with the posterior facet nearly out through the sole of the foot.
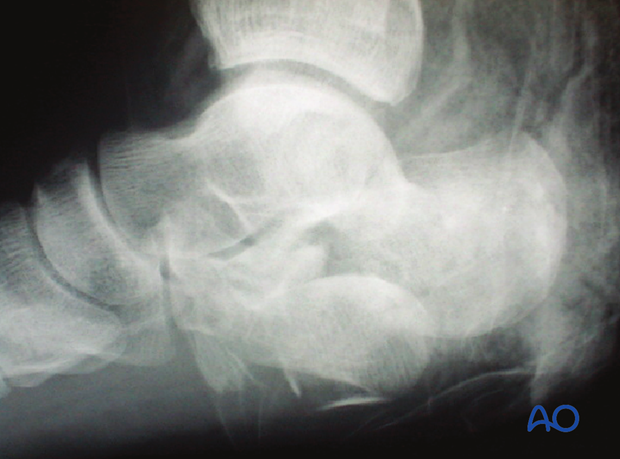
This image shows a severe open calcaneal fracture with antibiotic beads implanted, waiting for second debridement before definitive fixation.
Vacuum-assisted closure is also an excellent temporizing soft-tissue technique for severe foot injuries.
3. Definitive care
Principles of definitive care
The external fixator, or pinning, maintains bony stability for soft-tissue management. Once soft tissues are closed, or appropriate for surgery, definitive bony fixation is undertaken. Accurate reconstruction of joint surfaces with spanning plates over areas of marked comminution provide stability and enhance bony healing and soft-tissue care.
Foot shape and proper position of comminuted bone pieces is maintained by locking implants. This is one of the few places in the body where whole bones can be spanned if joints are accurately reconstructed.
Long spanning plates are best left in place for a period of months while the bony and soft-tissue injuries heal.
Management
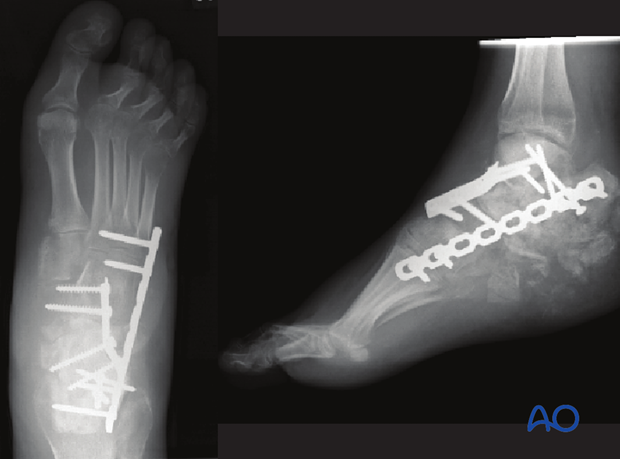
If the posterior facet is badly damaged, primary subtalar fusion is often the best form of treatment. Locking plates may also be used for added stability. Plate fixation across the hindfoot to the midfoot must be performed once the hindfoot-to-midfoot relationship has been restored to normal. One must avoid hindfoot varus, and medial, or lateral, column shortening.
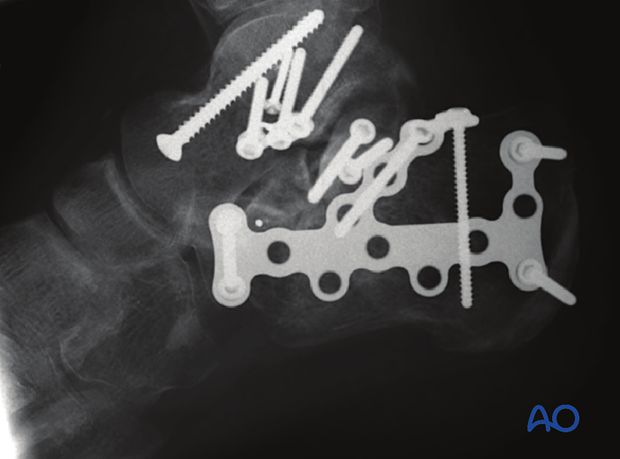
These images show a primary subtalar fusion carried out as a part of treatment of this massive talar and calcaneal injury.
4. Aftertreatment
Implant removal
Once all the fractures have healed, it may be necessary to remove the spanning plates which have been inserted across a number of joints.
This image shows a spanning plate from the calcaneus right to the forefoot.
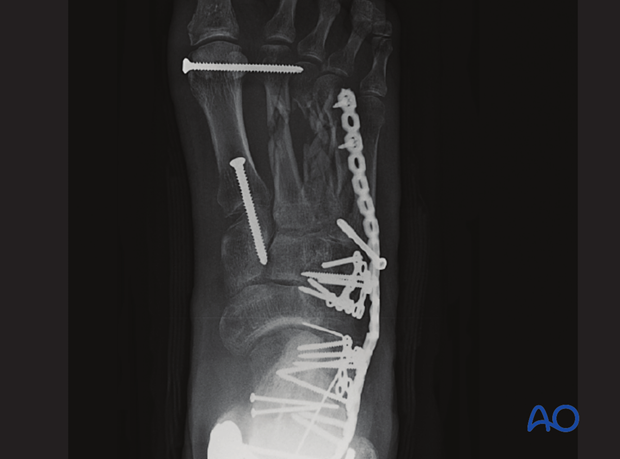
At three months, once the bony and soft-tissue injuries have healed, the plate was removed which allowed mobilization of the intervening joints.

Mobilization
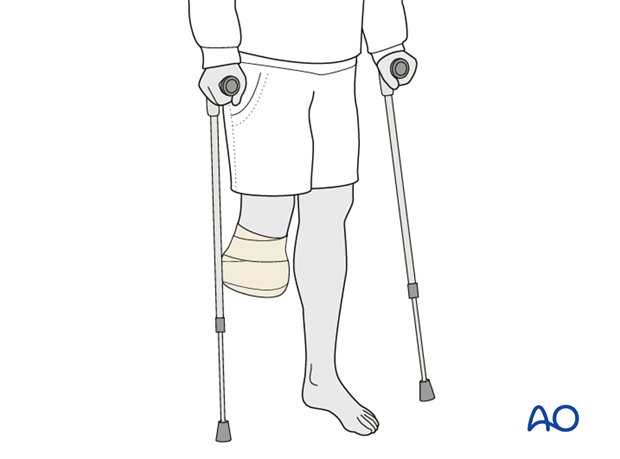
This image shows a young woman’s foot 3 months after severe hindfoot trauma. Mobilization is extremely important to achieve hindfoot and midfoot function after such serious injury. Subtalar stiffness occurs in virtually every patient but can be lessened by aggressive physiotherapy and aftercare.
Mobilization
Initially, the patient’s foot and ankle are kept in a well-padded posterior splint that maintains the foot in a neutral position. Surgical drains are removed 2 days after surgery.
The leg should be elevated intermittently through the first number of weeks. The ankle joint is put through range-of-motion exercises as soon as possible, or when soft tissues allow.
Weight bearing is delayed until 12 weeks.
Radiography including lateral and axial views is obtained at 6,12 and 26 weeks.
All patients with severe hindfoot trauma and combined injuries will require physiotherapy for optimal outcome.