Open reduction and preliminary fixation of lesser tuberosity and humeral head
1. Principles
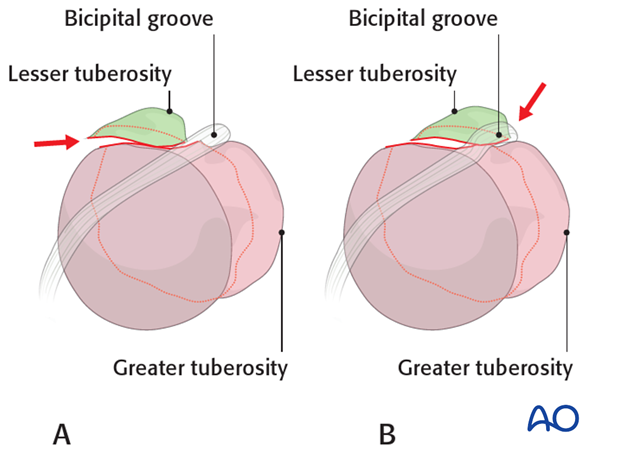
Lesser tuberosity reduction
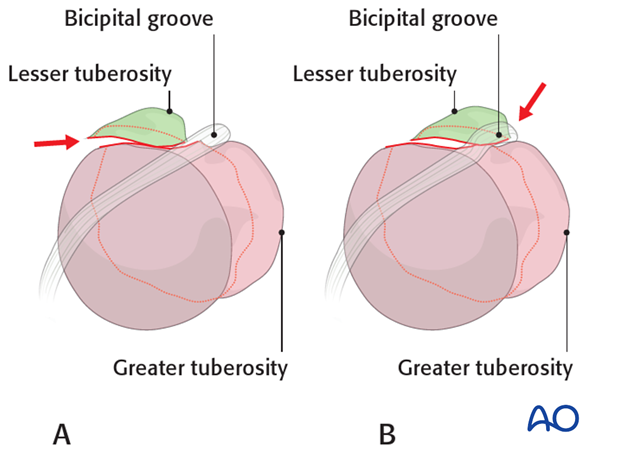
Proper reduction of the lesser tuberosity is difficult. Its position is hard to visualize with intraoperative image intensification.
Medial displacement of the lesser tuberosity (A) produces an intraarticular anterior step which can compromise internal rotation.
Lateral displacement of the lesser tuberosity (B) obstructs the bicipital groove and may compromise the biceps tendon. If possible, correct reconstruction of the bicipital groove is desirable to allow sliding of the tendon. An alternative would be tenodesis of the long head of the biceps.
The correct position of the lesser tuberosity is achieved if the fracture line between the lesser and the proximal humeral segment is closed precisely without any step or gap.
Proper reduction of humeral head segment
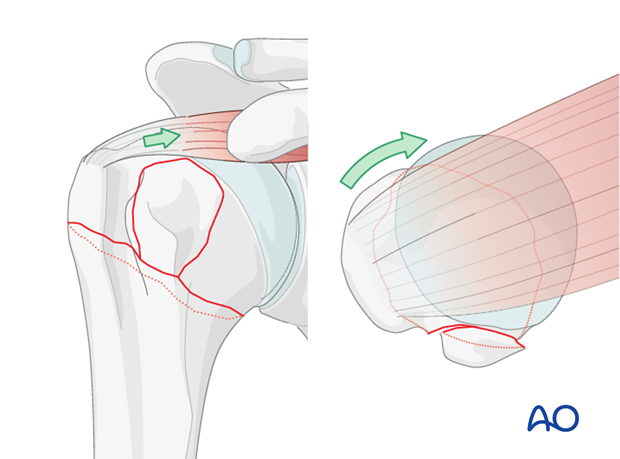
The humeral head with attached greater tuberosity is typically rotated externally and into a varus malposition due to the pull of the posterosuperior rotator cuff (supra- and infraspinatus tendons). This malposition of the humeral head should be reduced to allow for proper reduction of the lesser tuberosity (medial fracture line aligned).
2. Reduction and suture fixation of lesser tuberosity
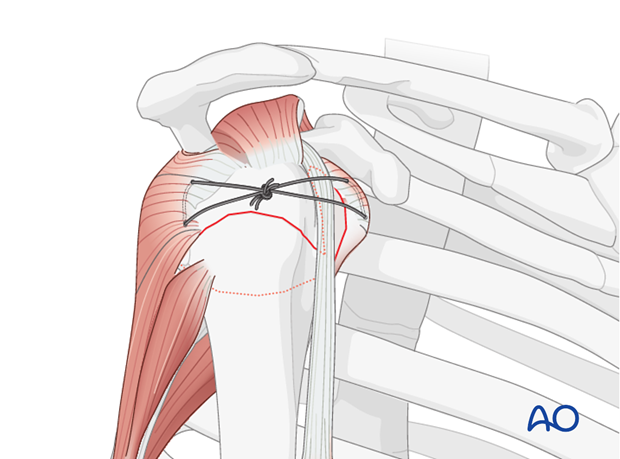
Sutures in the subscapularis tendon insertion aid both reduction and fixation of the lesser tuberosity. Once reduced, lesser tuberosity sutures are tied to a similar suture in the infraspinatus tendon for provisional fixation. Ultimately, these sutures contribute significantly to primary stability of the lesser tuberosity.
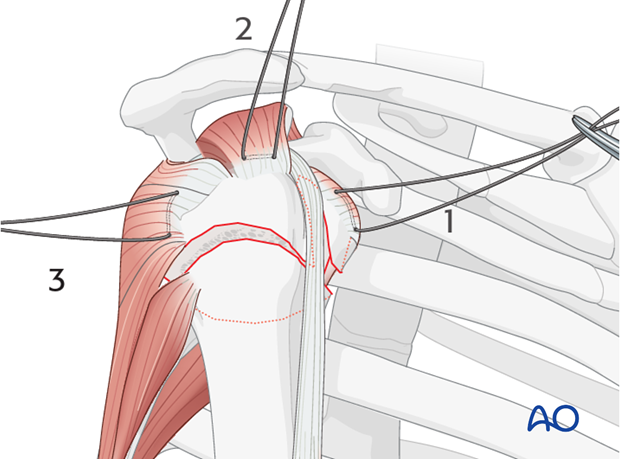
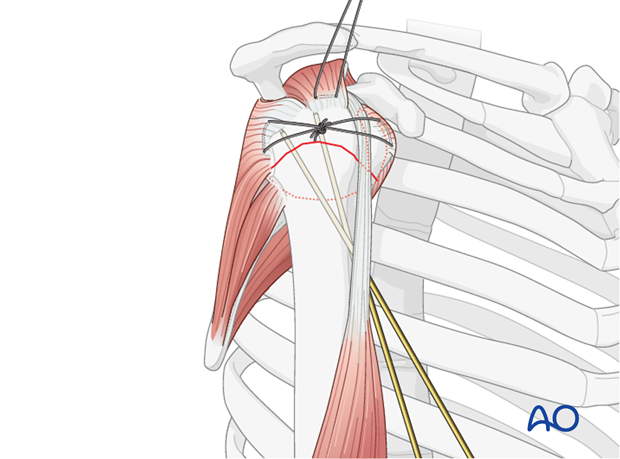
Placement of rotator cuff sutures
Subscapularis and supraspinatus tendon
Begin by inserting sutures into the subscapularis tendon (1) and the supraspinatus tendon (2). Place these sutures just superficial to the tendon’s bony insertions. These provide anchors for reduction, and temporary fixation of the greater and lesser tuberosities.
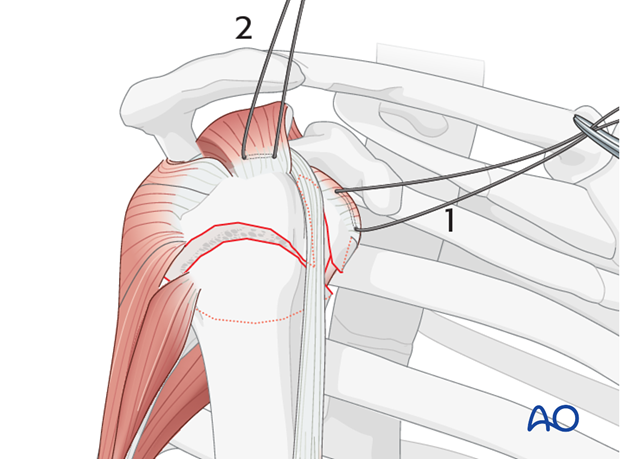
Infraspinatus tendon
Next, place a suture into the infraspinatus tendon insertion (3). This can be demanding, and may be easier with traction on the previously placed sutures, or with properly placed retractors.
Variations depending on the approach chosen
Inserting sutures into the infraspinatus tendon is easier with a lateral approach. A) shows a deltopectoral approach and B) an anterolateral (transdeltoid) approach.
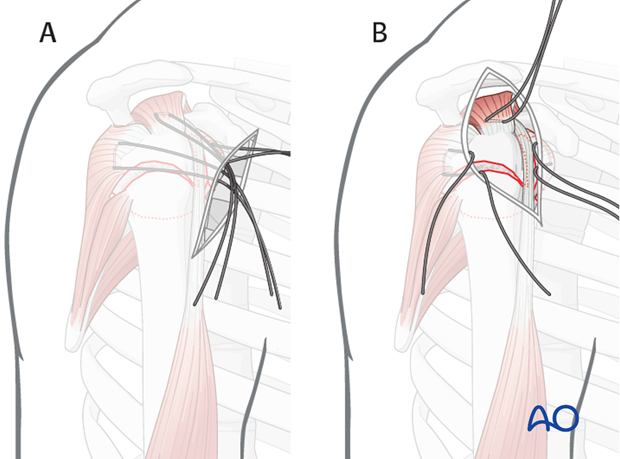
Use of stay sutures
Anterior traction on the supraspinatus tendon helps expose the greater tuberosity and infraspinatus tendon.
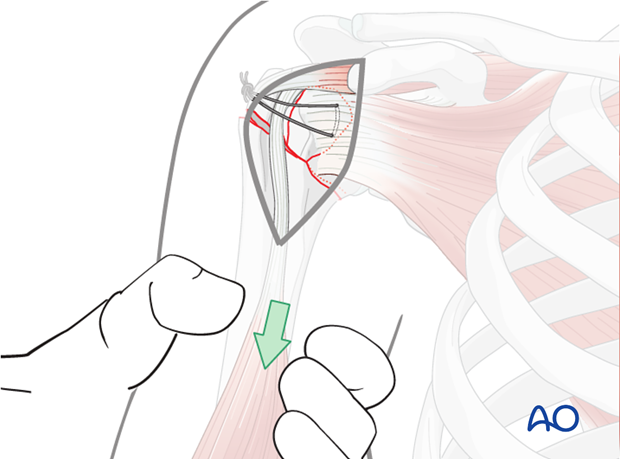
Insert a preliminary traction suture into the visible part of the posterior rotator cuff …
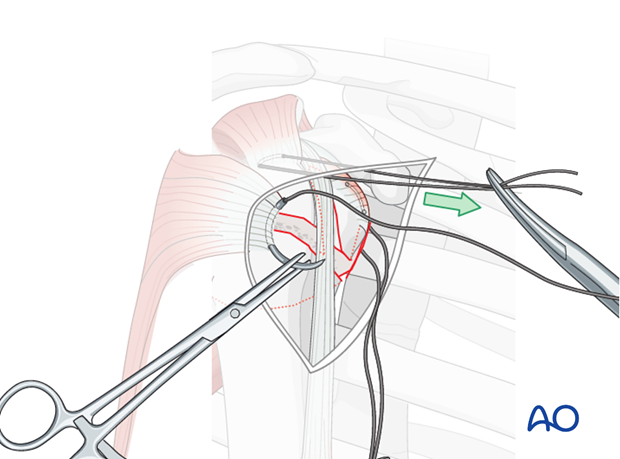
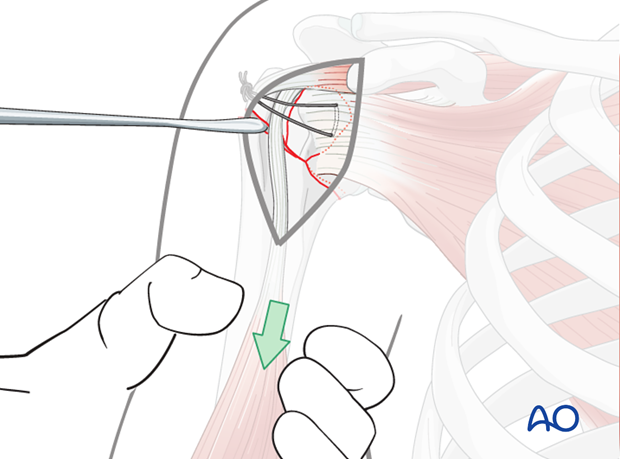
… and pull it anteriorly. This will expose the proper location for a suture in the infraspinatus tendon insertion. Then the initial traction suture is removed.
Pearl: A stout sharp needle facilitates placing a suture through the tendon insertion.
Pearl: Use of blunt, curved Hohmann retractors underneath the deltoid muscle can be helpful to expose the humeral head.
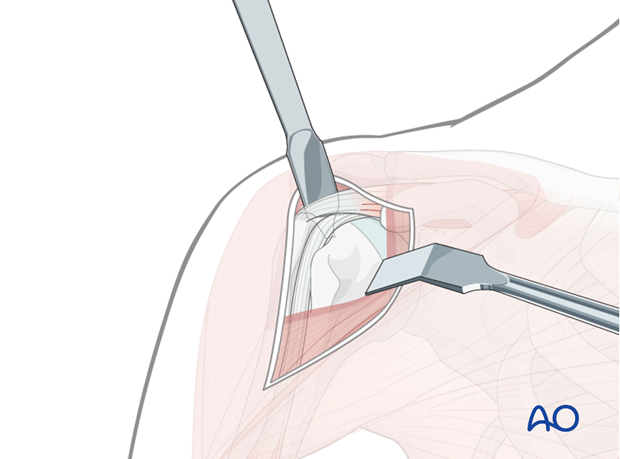
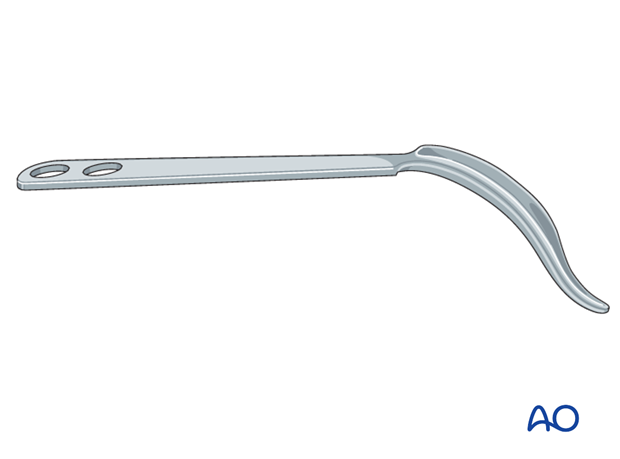
Similarly, a so-called delta retractor may improve deltoid retraction.
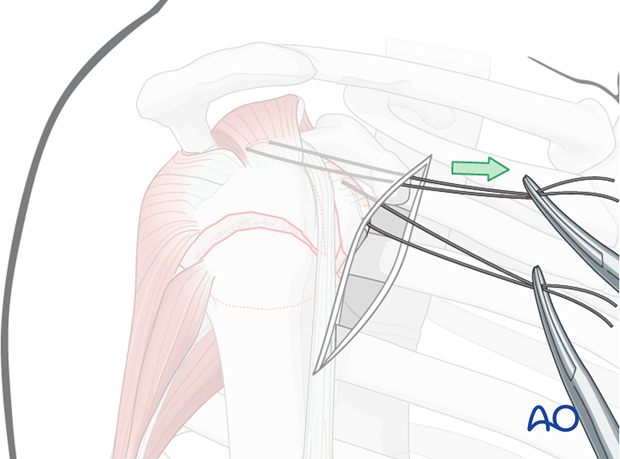
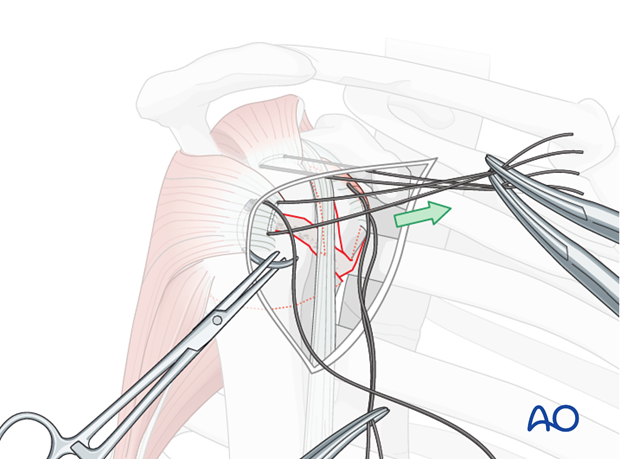
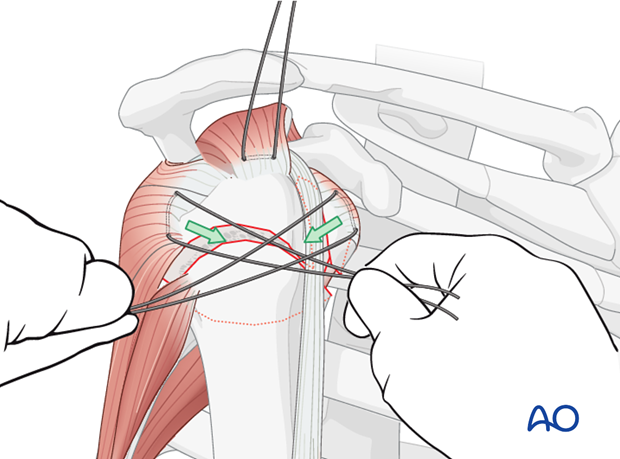
Reduction of lesser tuberosity
To reduce the lesser tuberosity, pull the sutures between the subscapularis and the infraspinatus horizontally.
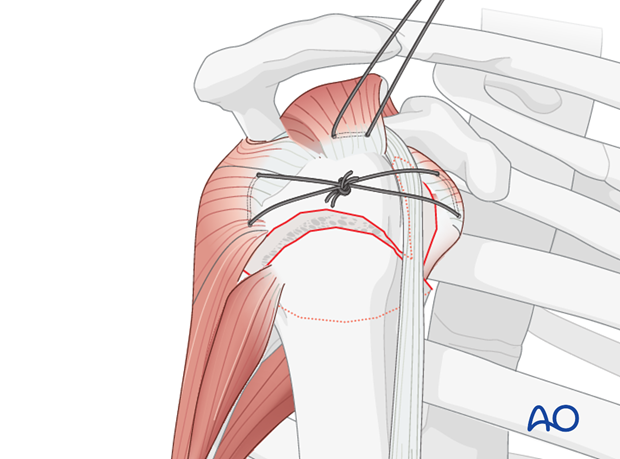
Preliminary fixation of lesser tuberosity
Tighten and tie the transverse sutures. Thus, reducing and fixing the lesser tuberosity to the proximal humeral segment converts the 3-part fracture into a 2-part situation.
In some cases, the lesser tuberosity is not mobile enough and therefore can not be reduced adequately. In this situation it is recommended to mobilize the lesser tuberosity using a periosteal elevator.
In some cases, due to the impacted head and displaced humeral head, there is not enough space for a proper reduction of the lesser tuberosity. In this situation, it is recommended to reduce the humeral head by disimpaction.
In cases of a multifragmentary lesser tuberosity it might become necessary to additionally fix single fragments with small K-wires.
Screw fixation of lesser tuberosity
If the stability of lesser tuberosity fixation is questionable, check it clinically by rotating the arm. If there is any micromovement visible or palpable consider additional fixation of the lesser tuberosity with lag screws or absorbable polymer pins.
3. Reduction and preliminary fixation of the head fragment
Reduction of metaphyseal fracture component
Since these fractures involve metaphyseal impaction, pure traction alone may not be effective to reduce the fracture.
While longitudinal traction is applied to the limb, a periosteal elevator can be inserted into the fracture gap to disimpact the fracture.
Preliminary fixation
After its reduction, the humeral head is preliminarily fixed to the shaft using two K-wires. Make sure to place them from anterior to avoid interference with the foreseen plate position.
4. Confirmation of reduction
After provisional fixation, confirm the correct reduction in both AP and lateral views using image intensifier control. Both humeral head segment and lesser tuberosity must be correctly positioned.
Confirmation of lesser tuberosity reduction
This can be very demanding.
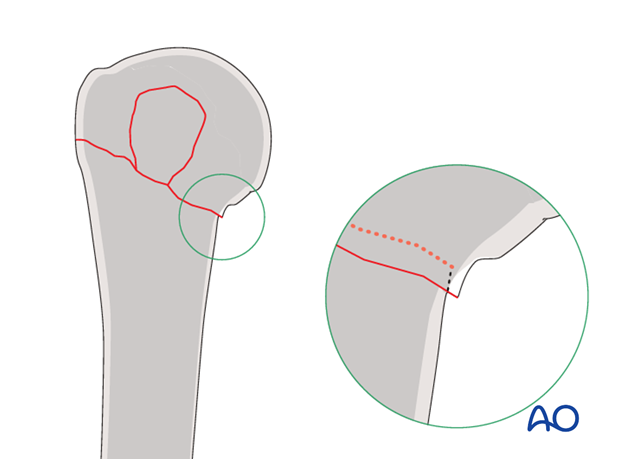
The lateral fracture line might be covered by the biceps tendon and the medial fracture line covered by the subscapularis tendon. Therefore, it is recommended to expose the lateral fracture line by slight removal of the periosteum to achieve visual control.
The lesser tuberosity is not visible in AP radiographic views, but is seen in profile on an axillary lateral view. Both projections should be assessed.
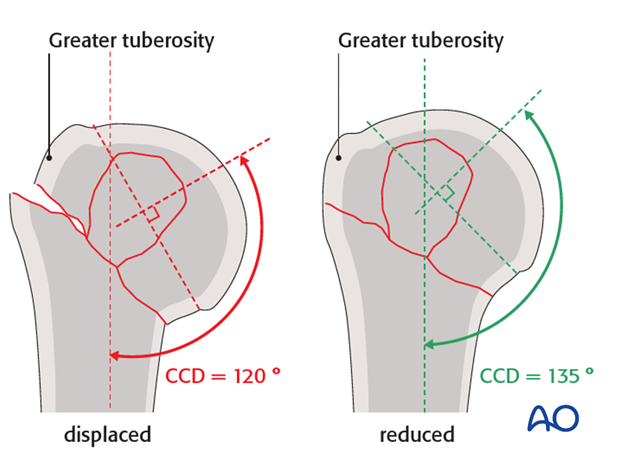
Confirmation of humeral head inclination
On the AP x-ray, confirm the correct inclination of the humeral head. The centrum column diaphyseal (CCD) angle should be 135°.
If the humeral head is still displaced, the reduction should be corrected since it may interfere with anatomic reduction of the lesser tuberosity.
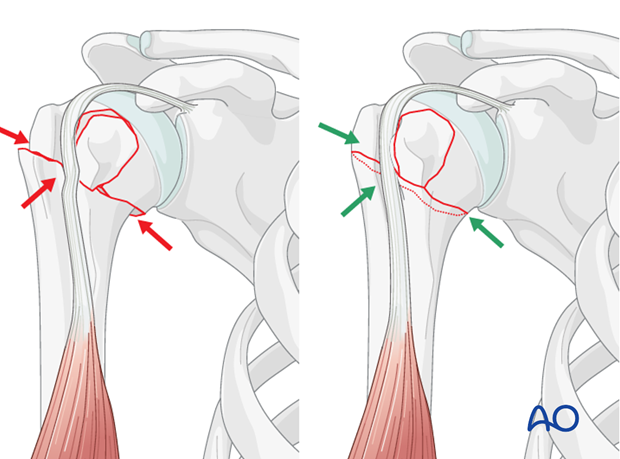
Confirmation of rotational alignment
Confirm correct rotational alignment by matching the fracture configurations on both sides of the fracture. This would be useful in the more transverse fracture configuration as shown in the illustration.
Pearl: Check retroversion. The bicipital groove might be a good indicator for correct rotation. In case of correct rotation, no gap/angulation is visible at the level of the fracture.
Remember that the humeral head is normally retroverted, facing approximately 25° posteriorly (mean range: 18°-30°) relative to the distal humeral epicondylar axis. This axis is perpendicular to the forearm with the elbow flexed to 90°.
Pearl: osteoporotic bone
In osteoporotic bone, stability may be increased by accepting some medial impaction of the humeral head.