Complications and technical failures in femoral neck fracture management
1. General considerations
Complications of the femoral neck fracture include:
- Nonunion
- Avascular necrosis
- Failure of fixation
2. Nonunion
Nonunion is caused by:
- Severity of the injury or displacement
- Shearing fracture configuration
- Inadequate reduction or
- Unstable internal fixation
Nonunion can be prevented by anatomical reduction and stable internal fixation.
In most cases, the fracture will displace into varus position.
If the blood supply to the femoral head is preserved, a valgus trochanteric osteotomy is a promising salvage procedure.
Case
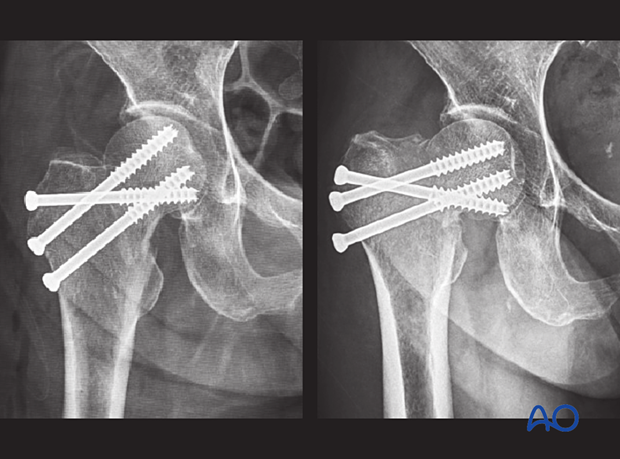
In this case, a basicervical femoral neck fracture was stabilized with multiple screws.

Postoperative AP and lateral views
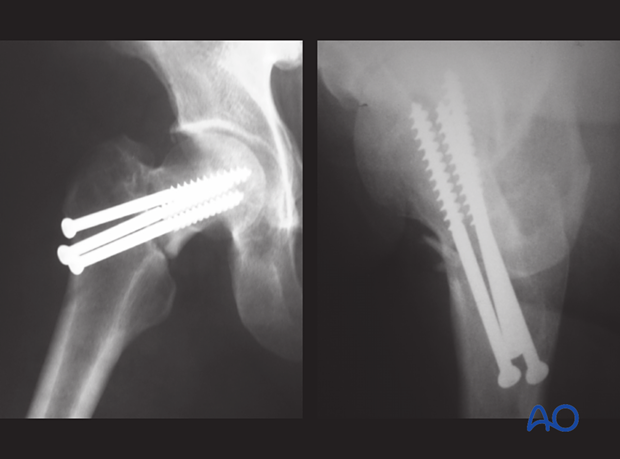
At 4 months follow-up, the fracture did not heal and displaced into varus deformity.
The nonunion was treated with valgus trochanteric osteotomy.
At 2 years, the femoral neck fracture healed, and the implant was removed.
3. Avascular necrosis
Avascular necrosis usually occurs in grossly displaced fractures. The vascular supply to the femoral head is jeopardized, especially the retinacular vessels.
Careful open reduction using an anterior approach will avoid iatrogenic injury to the blood supply of the femoral head.
Continued long-term follow-up is necessary since subchondral collapse due to avascular necrosis may take 2–3 years to become apparent on x-rays.
In most cases, it is treated with total hip arthroplasty.
Case
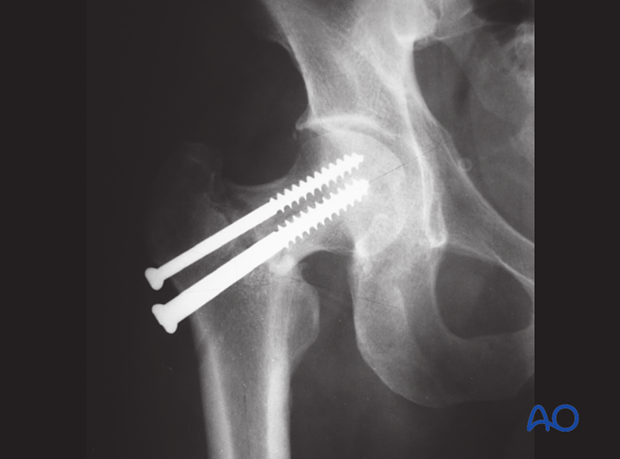
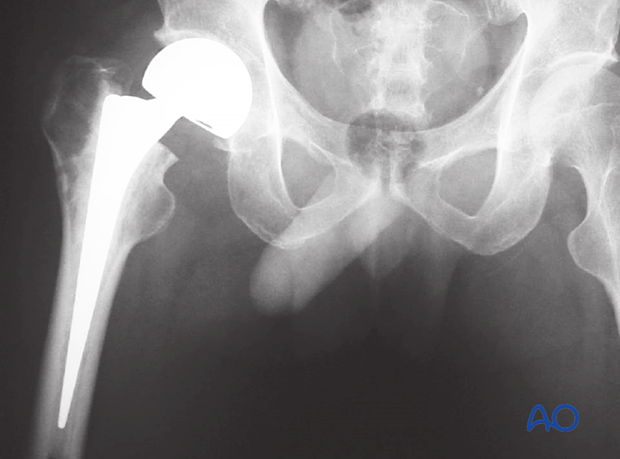
A transcervical femoral neck fracture was stabilized with multiple screws.
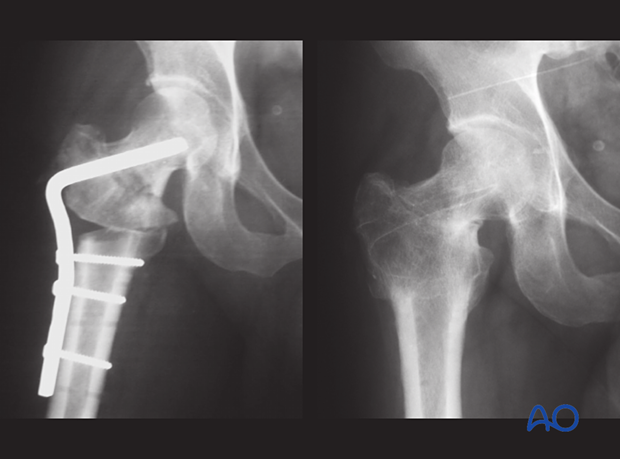
At six months, the fracture healed, but avascular necrosis with subchondral collapse occurred.
The final treatment was hemiarthroplasty.
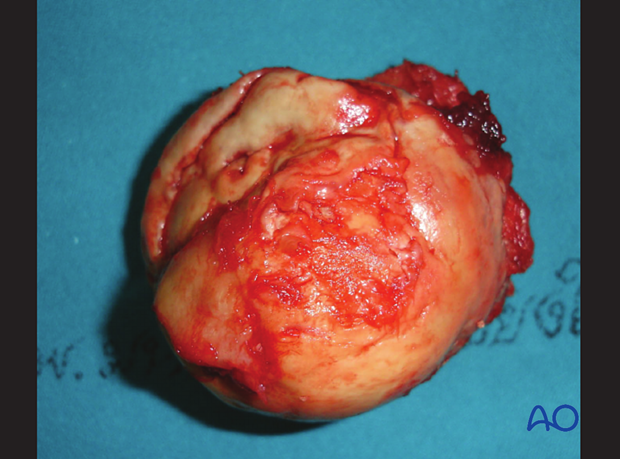
This image shows the condition of the articular cartilage of the femoral head with partial collapse.
4. Failure of fixation
In poor-quality bone
Failure of fixation is related to poor bone quality, especially in elderly patients with osteoporosis. Fixation of a displaced femoral neck fracture in osteoporotic bone usually ends up with implant loosening or loss of fixation.
Careful evaluation of the x-rays is necessary to determine whether the fracture is nondisplaced or displaced.
If there is displacement, attempts for anatomical reduction and internal fixation often lead to failure of fixation. Arthroplasty is the preferred choice in this case.
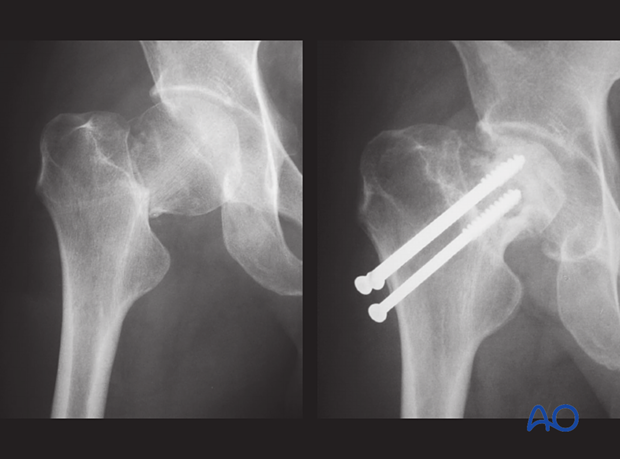
Case
This case shows a transcervical fracture of the femoral neck in an elderly patient with osteoporosis.

It was reduced closed and stabilized with multiple screws.
At 6 weeks follow-up, the fracture displaced and collapsed into varus.
In good-quality bone
In young adults, failure of fixation is mainly related to technical errors. The quality of reduction is the most important factor in predicting healing (or implant failure).
Unstable fracture configurations, eg, shearing fracture types, need more stable implants, eg, sliding hip screw combined with an antirotation screw, or the femoral neck system (FNS).












