Modified stoppa to the anterior intrapelvic region
1. Introduction
This approach was first described by Hirvensalo et al in 1993. A similar approach "Modified Stoppa" was described in 1994 by Cole et al.
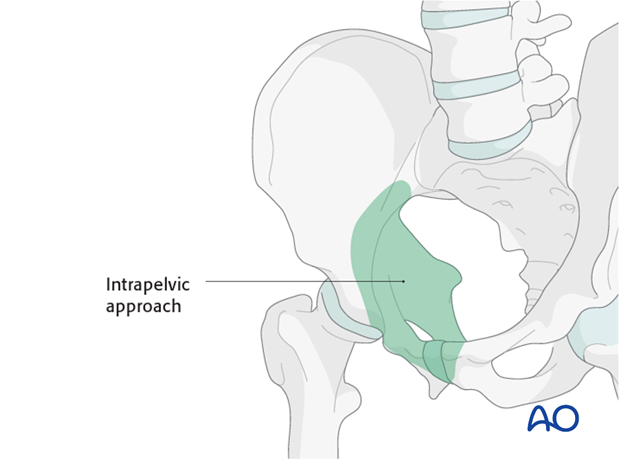
It can be used to access anterior fractures of the pelvic ring as far laterally as the acetabulum.
This approach to the anterior intrapelvic region allows visualization of:
- The entire symphysis
- Both pubic bodies
- The complete superior pubic ramus
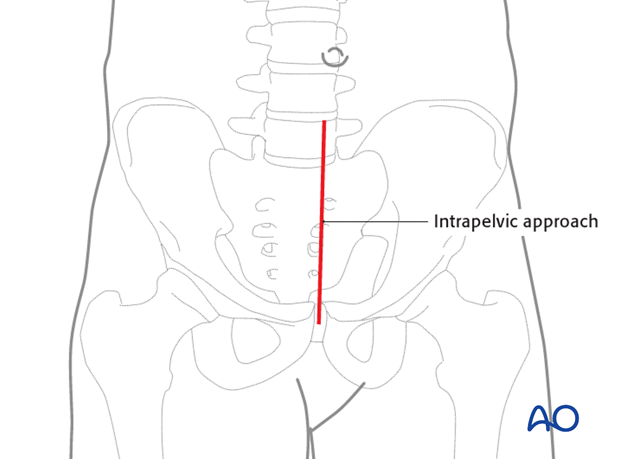
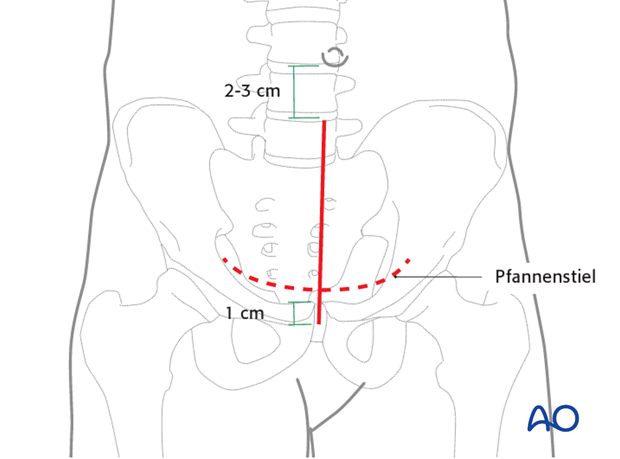
2. Skin incision
A midline skin incision is made starting 1cm inferior to the symphysis and ending 2-3 cm inferior to the umbilicus. Occasionally, a Pfannenstiel incision can be used.
3. Deep dissection
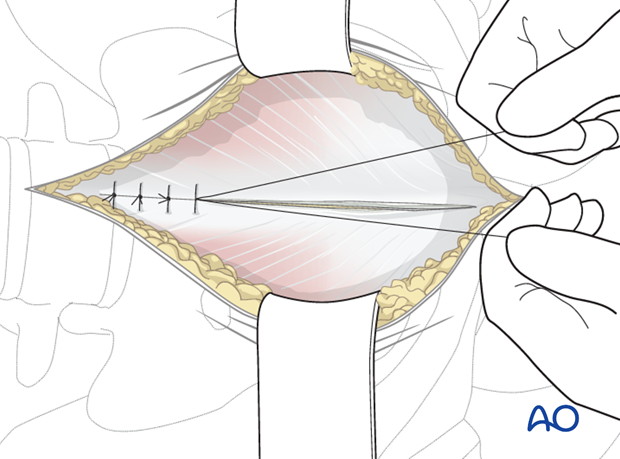
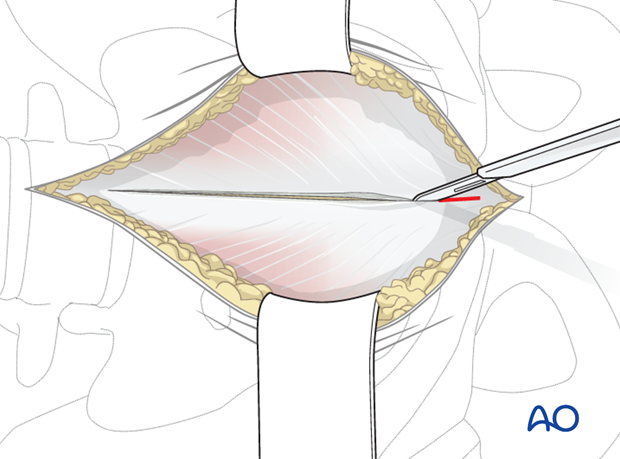
Divide the subcutaneous tissues in line with the skin incision in order to expose the fascia overlying both rectus muscles of the abdomen.
The rectus fascia is incised in longitudinal fashion along the linea alba.
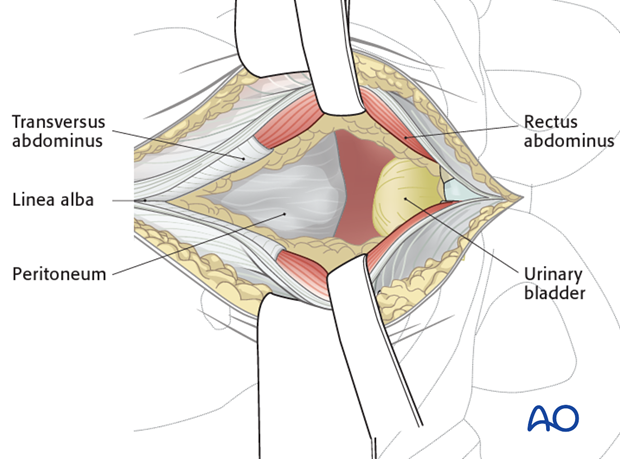
Both bellies of the rectus abdominis muscle are gently retracted laterally.
The fascia between the heads of the rectus muscle is identified. In nearly all cases, this fascia has been disrupted by the injury. The surgeon can use the resulting defect in the fascia as a starting point for blunt dissection.
In the proximal part of the incision, care should be taken not to incise the peritoneum. The entire approach should stay in the pre peritoneal space.
A wet sponge is loosely packed in the retropubic space to protect the urinary bladder.
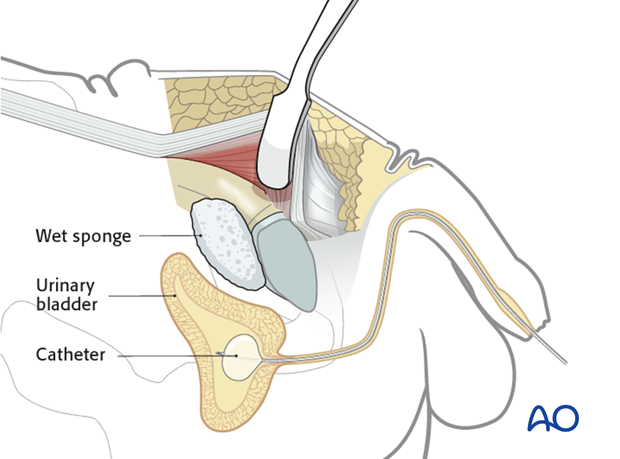
The medial part of the rectus muscle is partly detached from the upper and anterior part of the symphysis.
The thick periosteum from the superior pubic bone is dissected sharply, allowing for deeper blunt dissection.
At the beginning, dissection should be enlarged also on the anterior part of the symphysis.
The upper border of the superior pubic ramus is identified (pecten pubis) and the dissection is carried laterally along the pelvic brim. The iliopectineal fascia is detached from the pelvic brim.
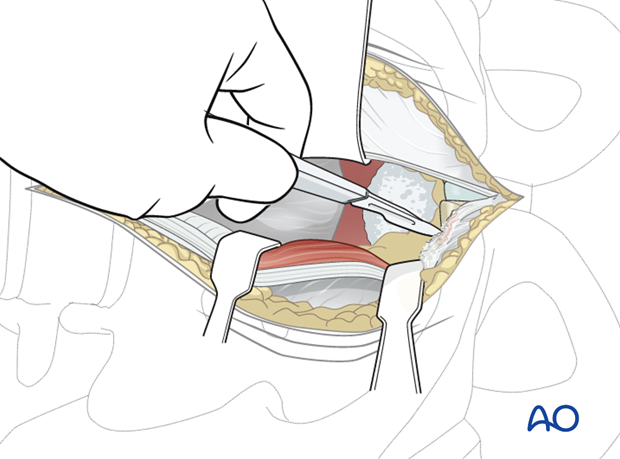
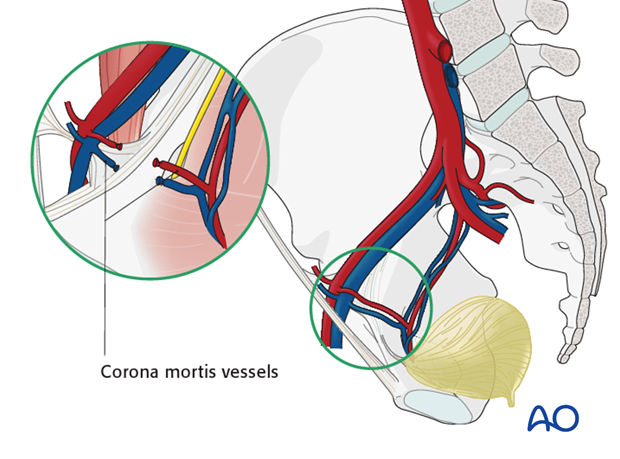
Dissecting carefully along the medial surface of the superior ramus, the corona mortis vessels are identified and ligated (or clipped) as necessary.
Dissection of the periosteum is continued further laterally following the upper border of the superior pubic bone to the direction of the pelvic brim exposing the beginning of the iliopectineal eminence.
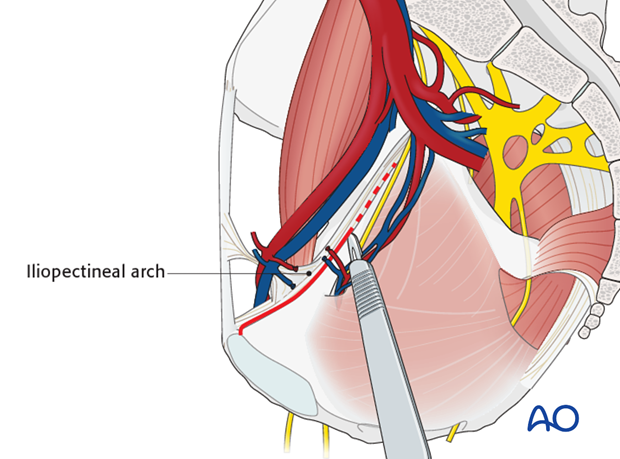
At this point the beginning of the iliopectineal arch should be dissected from the bone. This enables the elevation of the femoral vessels and nerve.
The dissection is continued subperiosteally more laterally following the upper border of the pelvic brim.
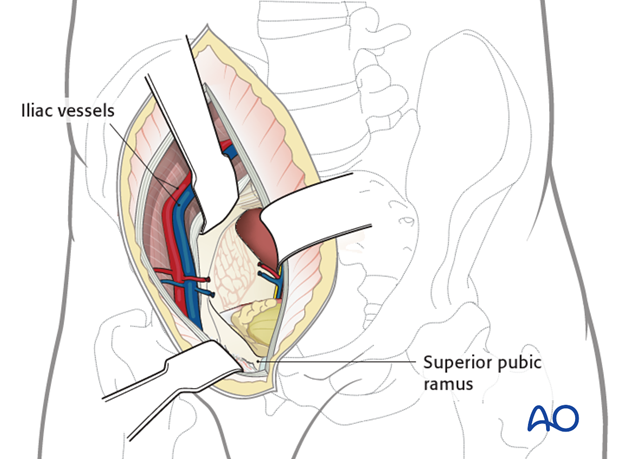
At this point the entire internal surface of the superior pubic ramus has been exposed adequately for plate fixation.
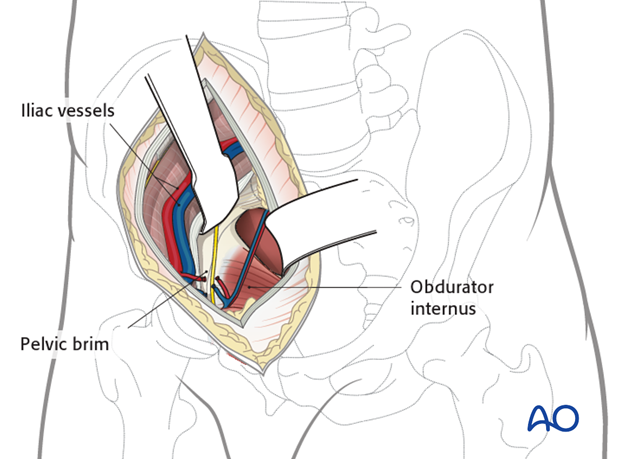
At this level, the obturator neurovascular bundle is crossing the quadrilateral surface. In some cases it should be mobilized. A spatula or malleable retractor is used to protect the obturator neurovascular bundle and pelvic floor.
With a Cobb elevator, the periosteum and obturator internus is elevated and the quadrilateral surface can be sufficiently exposed.
One Hohmann retractor should be put in the middle part of the superior pubic ramus and another curved Hohmann retractor is placed on the posterior top of the acetabulum on the iliac part of the pelvic brim.
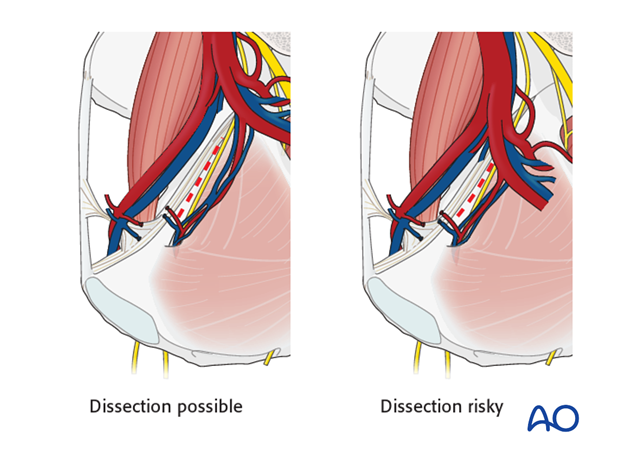
Great care should be taken not to injure the external iliac vein which may be in close proximity to the elevators.
In some rare cases, the internal iliac artery bifurcates very distally and makes the dissection of the posterior part of the quadrilateral surface risky and limits the further dissection.
4. Closure
The intrapelvic space may be drained.
The midline incision in the rectus abdominis and superficial tissues are closed in layers.