Compartment syndrome of the foot
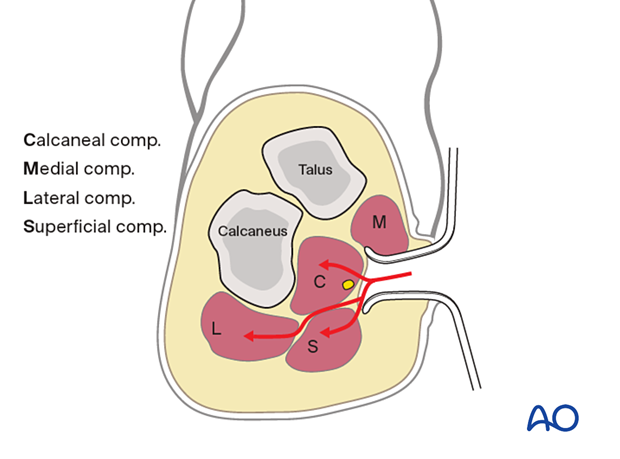
1. Compartments in the foot
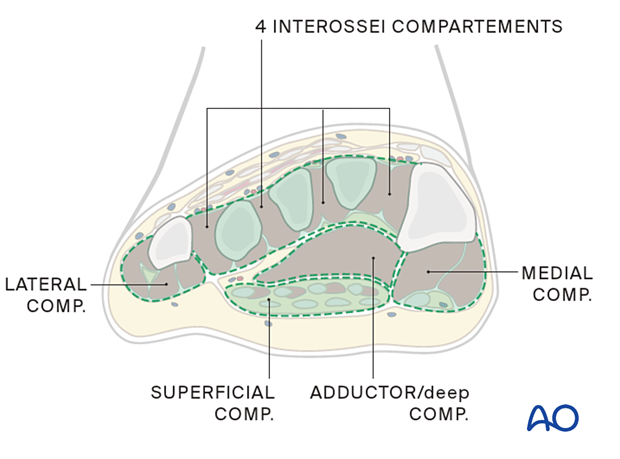
There are several foot compartments; these may include:
- Medial
- Superficial
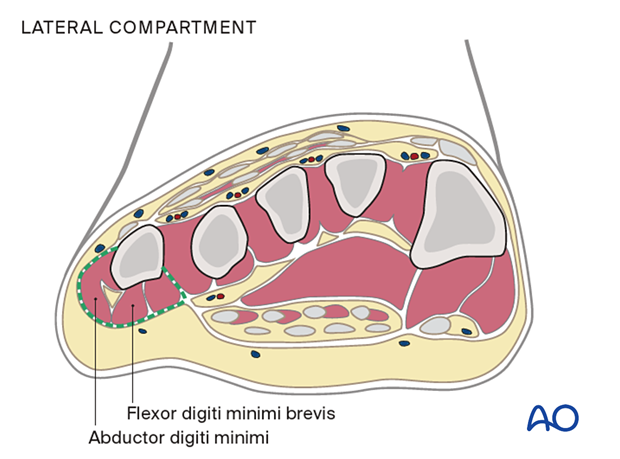
- Lateral
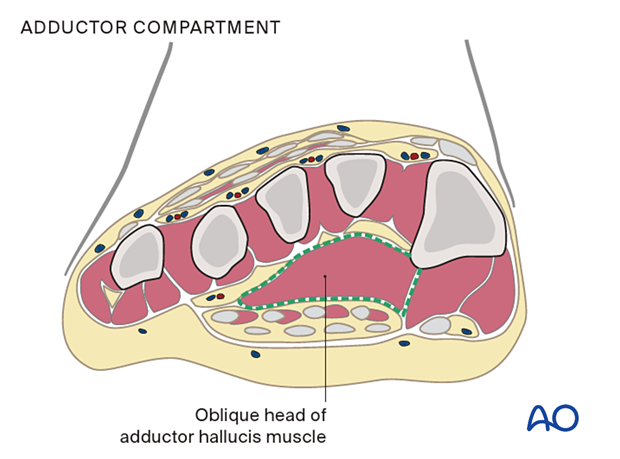
- Adductor
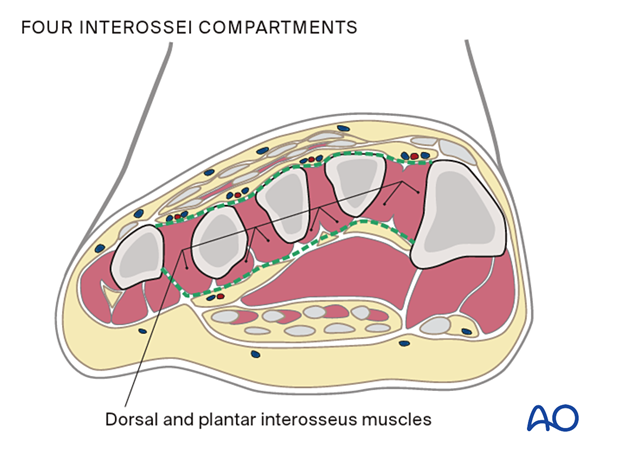
- Four interossei
- Calcaneal
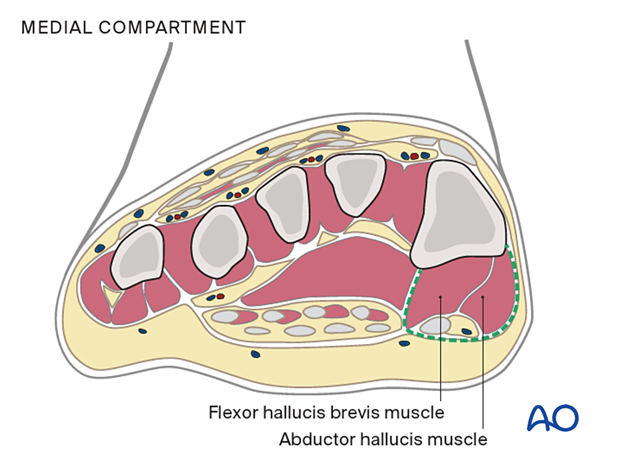
The medial compartment contains the abductor hallucis and flexor hallucis brevis muscles and is plantar-medial to the first metatarsal.
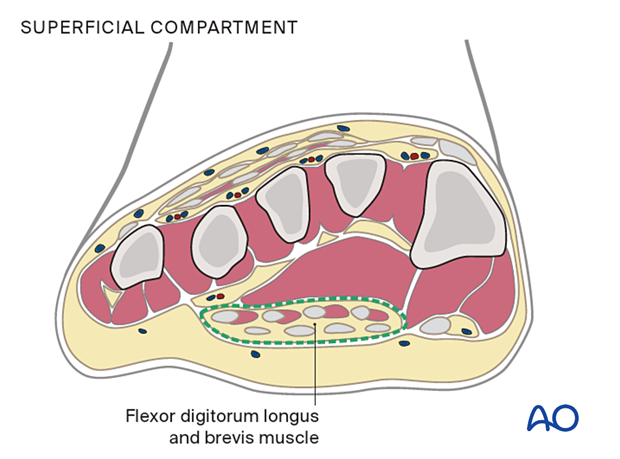
The superficial compartment contains the flexor digitorum longus and brevis muscles.
The lateral compartment contains the abductor digiti minimi and flexor digiti minimi brevis, and is on the inferolateral surface of the fifth metatarsal.
The adductor or deep compartment is located in the plantar forefoot, containing the oblique head of the adductor hallucis muscle.
The four interossei compartments are dorsally located between the metatarsals, and each includes dorsal and plantar interosseus muscles.
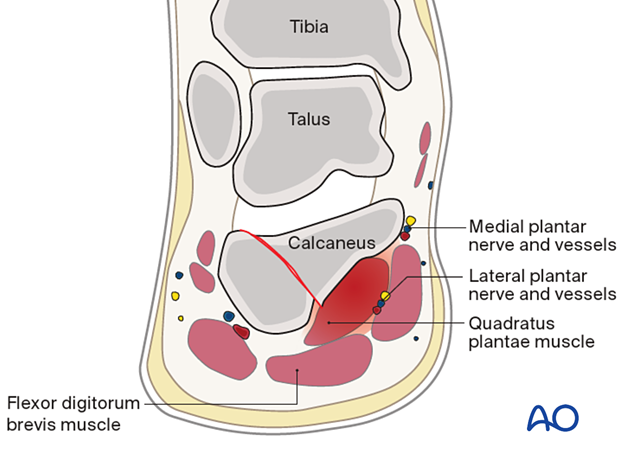
The calcaneal compartment contains the quadratus plantae muscle.
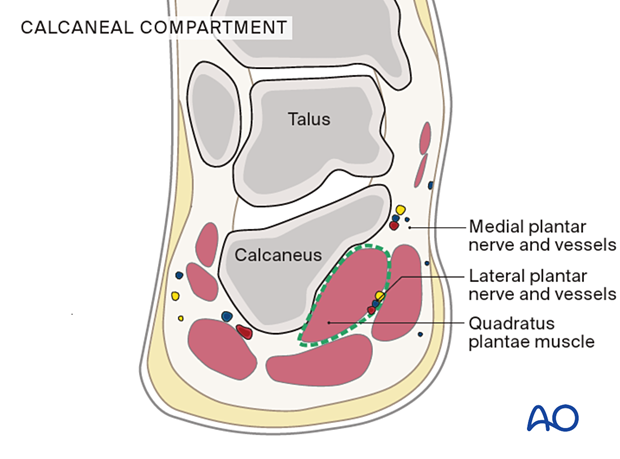
In calcaneal fractures, the sustentacular calcaneal fragment causes bleeding from the bone or the medial calcaneal arteries into this compartment. The medial and lateral plantar nerves and vessels are then compressed between the quadratus plantae and the short flexor digitorum muscles (flexor digitorum brevis).
2. General considerations
In summary, foot compartment syndrome can lead to complications. Early suspicion and treatment may prevent this from happening. Compartment syndrome is a clinical diagnosis, and treatment should not be delayed if a measuring tool is not immediately available. Open incision release may be considered, with the downsides being possible infection, need for soft tissue coverage, and the need for future cosmetic scar revision.
If compartment syndrome of the foot is missed or left untreated, long-term surgery may be needed to reconstruct or release intrinsic toe contractures. Compartment syndrome affecting some foot compartments may leave minor sequelae only, such as claw toes or hammer toes. A debate exists in the literature and among trauma and foot experts about the efficacy of compartment releases.
After the fasciotomies are performed, metatarsal fractures can be fixed with small plates and screws. Occasionally, Kirschner wires are helpful. Lisfranc joint injuries can be fixed with screws using standard techniques.
The problem is that these wounds cannot be closed and must be left open, often with metal in their depth, with considerable risk of infection.
3. Specifics of diagnosing compartment syndrome in the foot
Diagnosis of compartment syndrome in the foot is primarily a clinical diagnosis with a need for high suspicion.
In these foot injuries, the usual signs of increased local pain, decreased sensation, or passive stretch pain in the foot is often unreliable.
Tense swelling and severe pain are the hallmarks of an impending compartment syndrome; the most consistent physical finding is tense foot swelling. The treatment may be decompression without delay.
There is no clinical tool that allows a surgeon to know whether or not a compartment syndrome in the foot can be salvaged safely with a surgical release.

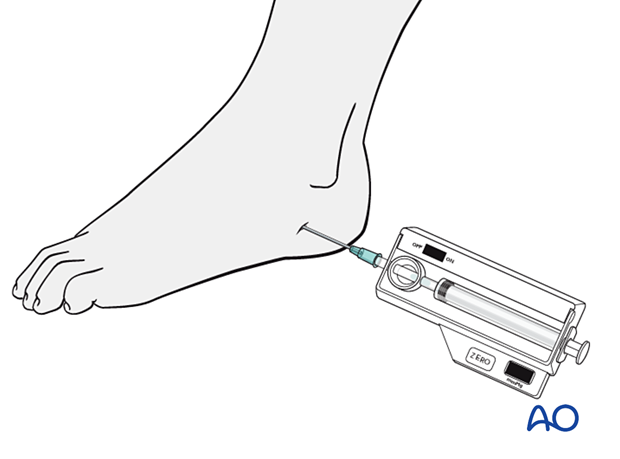
Compartment pressure monitoring is a practical confirmatory test. There are compartment pressure measuring devices that are commercially readily available.
Measurement of the affected compartments is difficult. The compartments involved are usually adjacent to the areas of injury but may be more remote.
The threshold for considering compartment syndrome and performing fasciotomy must/should be high.
Acute dermato-fasciotomy of any nine compartments may be indicated when compartment pressure exceeds 30 mmHg or if compartment pressure is more than 10- 30 mmHg less than the diastolic pressure.
Normal pressures in the foot are 5 +/- 3 mmHg, with a range of 1 to 12 mmHg.
It is essential to reach the calcaneal compartment when involved (in the case of hindfoot trauma), as it appears to be the most sensitive.
Surgeons dealing with this problem must be cognisant that potential treatment is not worse than the end result of the syndrome itself.
4. Treatment principles
Approaches
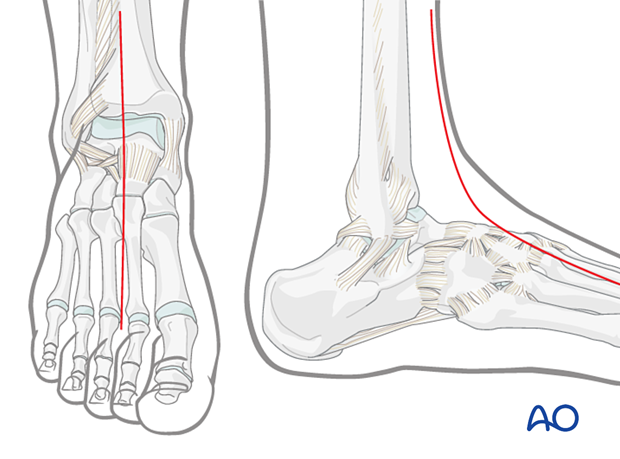
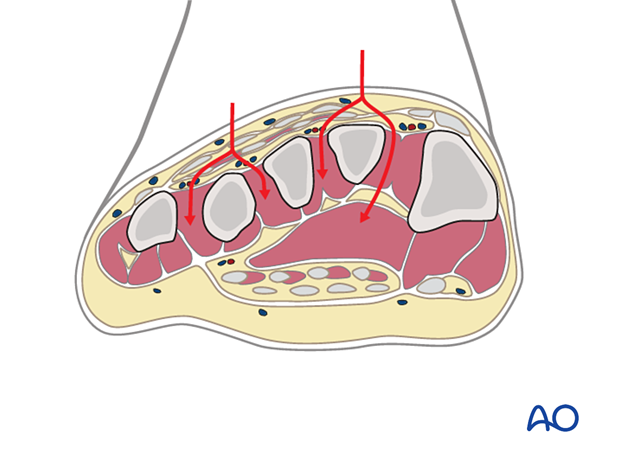
The release of compartment syndrome of the foot is very much debated in the literature. If performed, the approaches for compartment decompression generally include two dorsal incisions for access to forefoot/interossei compartments, one medial incision for decompression of the calcaneal, medial, and superficial compartments, and one lateral incision for the lateral compartments.
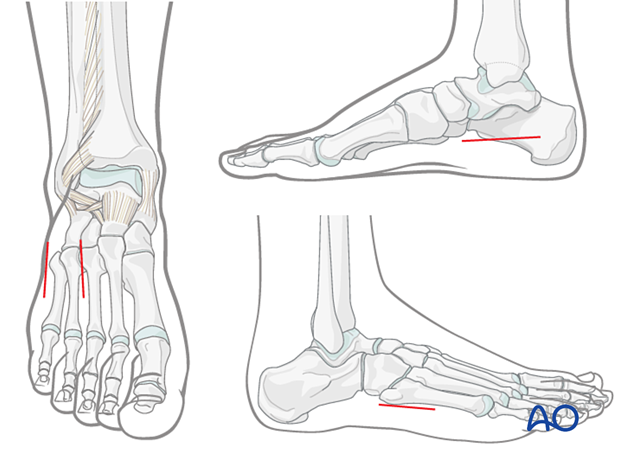
An alternative incision, which is helpful, especially in severe trauma for foot and leg salvage, starts at the base of the second toe and progresses to the mid-ankle region. It then ascends the leg over the anterior compartment.
In cases of severe leg trauma or crush injury, a more thorough decompression is possible all the way up to the knee. To reach the superficial and deep compartments of the lower leg, one must undermine the soft tissue flap on the medial side.
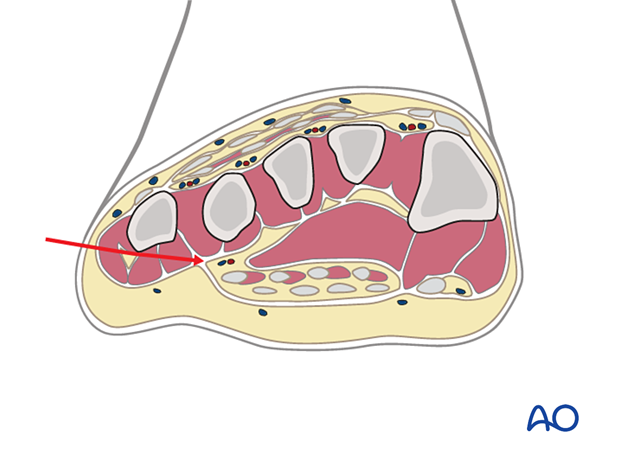
Double-dorsal incision
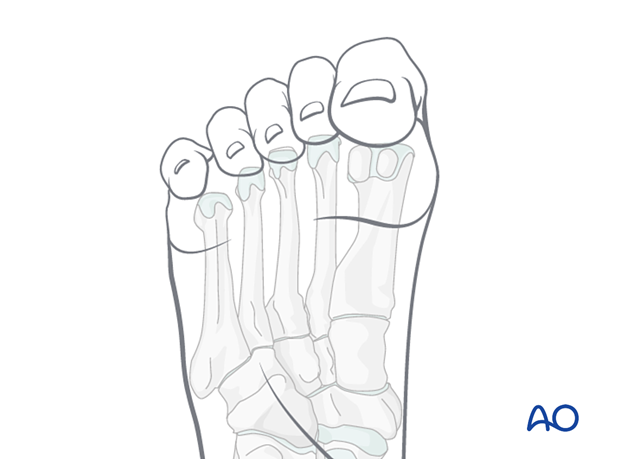
The two dorsal incisions are placed, one medial to the second metatarsal shaft and one lateral to the fourth metatarsal shaft.
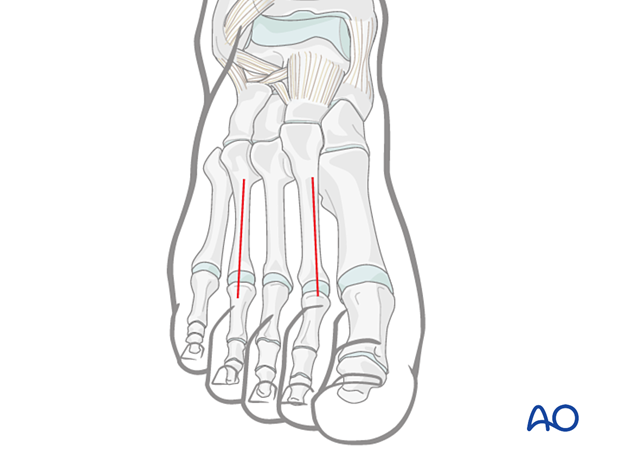
The fasciae of the interosseous muscles are opened dorsally. The muscle is stripped off the second metatarsal medially, and the fascia of the adductor compartment is opened bluntly deep within the first interspace.
Medial incision
The medial incision is made within the foot's arch, along the muscle body of the abductor hallucis.
Dissection is continued both dorsal and plantar to the abductor hallucis muscle, which disrupts the superficial and deep components of the central compartment and allows access to the adductor muscle belly.
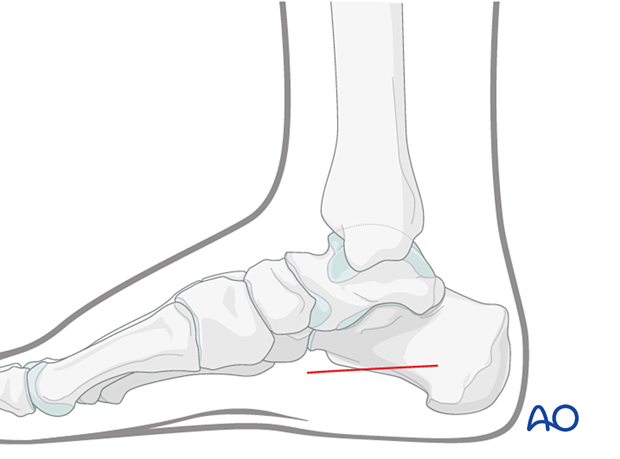
Lateral incision
The lateral incision is made immediately plantarward of the fifth metatarsal and should be about 4 cm in length.
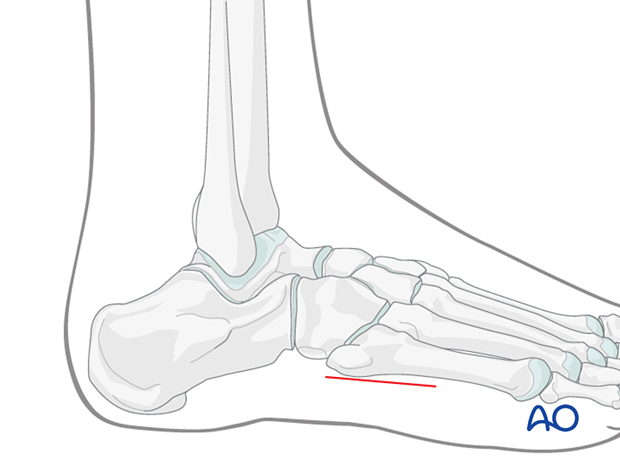
The abductor digiti minimae compartment is released.
5. Prognosis
Long-term sequelae of foot compartment syndrome (FCS) may include contractures, deformity, weakness, paralysis, and sensory neuropathy. Mild compartment syndrome of the foot may leave very minor sequelae only. A debate exists in the literature and among trauma and foot experts about the efficacy of compartment releases.
Claw toe deformity following calcaneus fracture appears to be due to late contracture of the quadratus plantae muscle in the calcaneal compartment.
Since it can communicate with the deep posterior compartment of the leg, compartment syndrome of the calcaneal compartment can lead to significant deformity of the foot and toes. If the posterior tibialis musculotendinous unit necroses or dies, it can lead to equinocavovarus deformity.

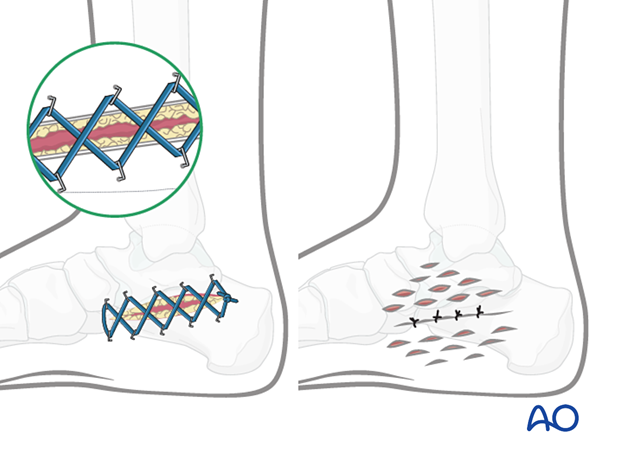
6. Aftercare
Fasciotomy wounds may require delayed primary closure (left), negative pressure device (NPWT), pie crusting (right), or skin grafting.
Late reconstruction in the presence of subsequent deformity includes:
- Excision of scarred muscle, tenotomies, and correction of structural deformities with tendon transfers and rebalancing.
- Providing a plantigrade foot without static structural deformity.
- Providing the patient with the possibility of wearing standard shoeware.
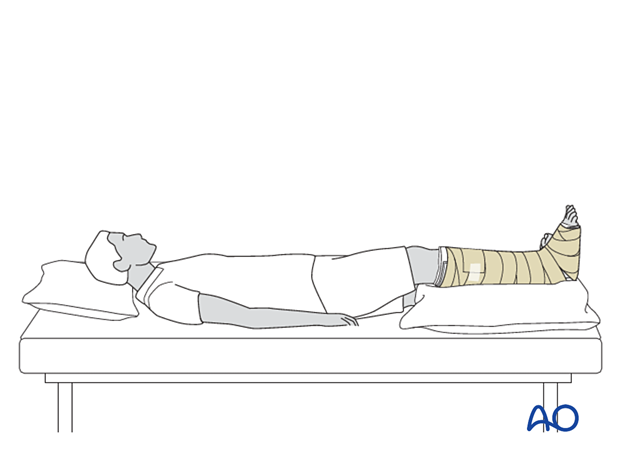
Once the wounds are appropriately dressed, provide posterior splinting to prevent equinus deformity from developing.
If the foot is badly swollen, the patient must be supine, and the extremity must be elevated so that the foot is higher than the heart.