Patient assessment
1. Introduction
Hand surgery involves a multi-specialty approach to the assessment, treatment, and aftercare of hand trauma. Therefore, the specialized teams should be involved early on according to the specific injury requirements.
A diagnosis is made based on the history, the mechanism of the trauma, clinical examination, and by x-rays in two planes.
2. Clinical assessment
Check for:
- Swelling
- Open wound
- Loss of sensation in the fingers (indicating nerve injuries)
- Perfusion (reperfusion of more than 2 seconds may indicate vascular injuries)

General assessment of hand and wrist
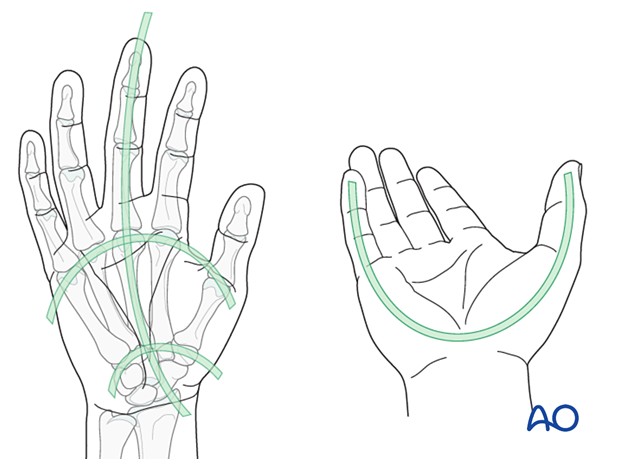
Check for anatomical architecture (position and relation) of the whole hand:
- Longitudinal arc
- Metacarpal arc
- Oblique arcs (with thumb in opposition)
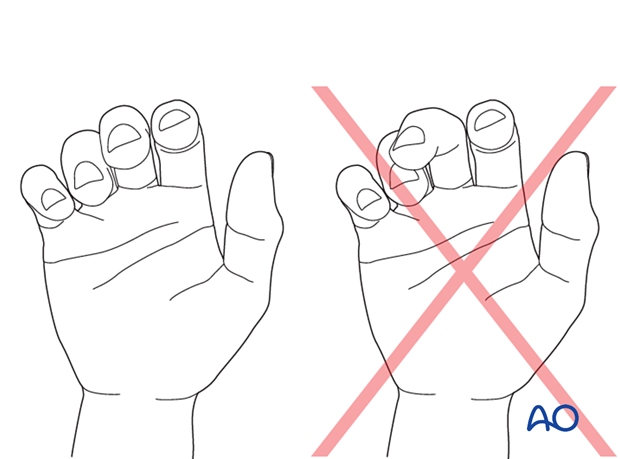
The tips of the flexed fingers should point to the scaphoid. Check for deviating or overlapping fingers. This will indicate malrotation.
Assessment of the metacarpals
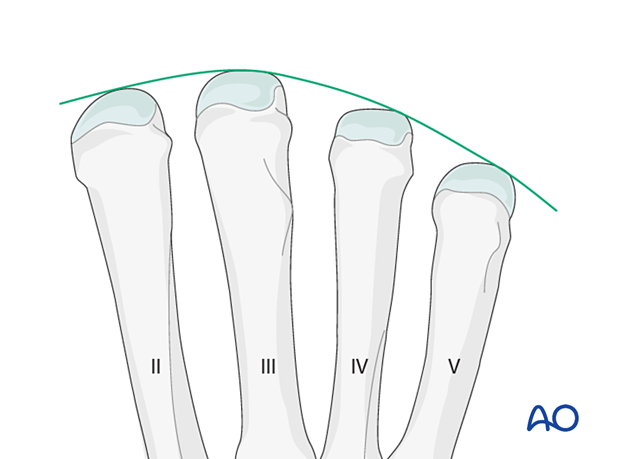
Check for shortening of a finger. An interrupted arch of the metacarpophalangeal (MCP) joints indicates shortening.
Check for deformity of a metacarpal and dislocation of proximal and distal joints.
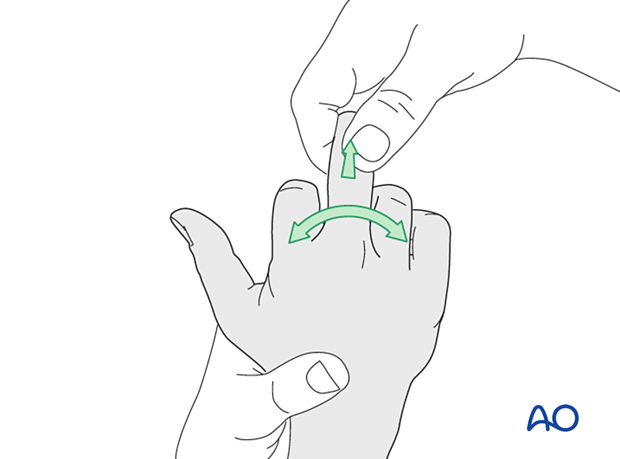
Check the MCP joint stability. Compare it with the contralateral finger.
Lack of lateral stability indicates injury of the collateral ligaments or their bony attachments.
3. Radiologic evaluation
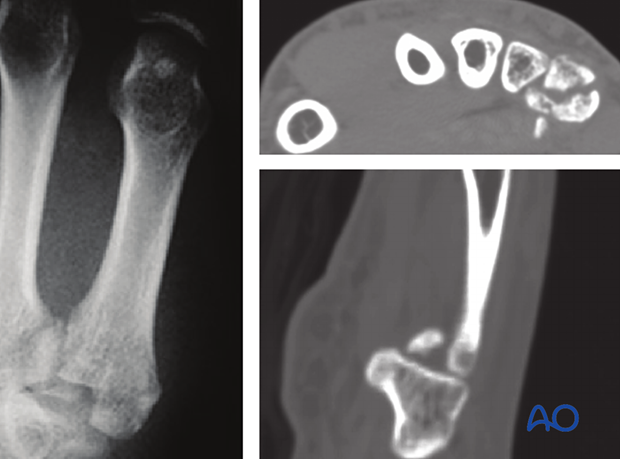
X-rays
AP, oblique, and lateral views of the whole hand are needed for diagnosis.
All views need to be inspected to get information about the fracture pattern, eg, the orientation of an oblique fracture plane.

Be aware of fracture lines/extensions not visible in a preoperative X-ray, especially in high-energy trauma.
CT imaging is very helpful in such cases to evaluate the fracture complexity and plan treatment accordingly.
CT imaging
CT imaging is required in complex cases with articular compromise.
MRI
Ligamentous injuries may be seen in an MRI.












