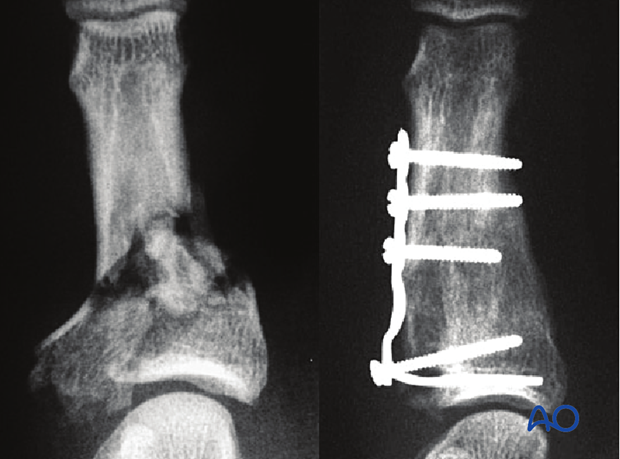
Minicondylar plate fixation of Pilon compression fracture
1. Principles
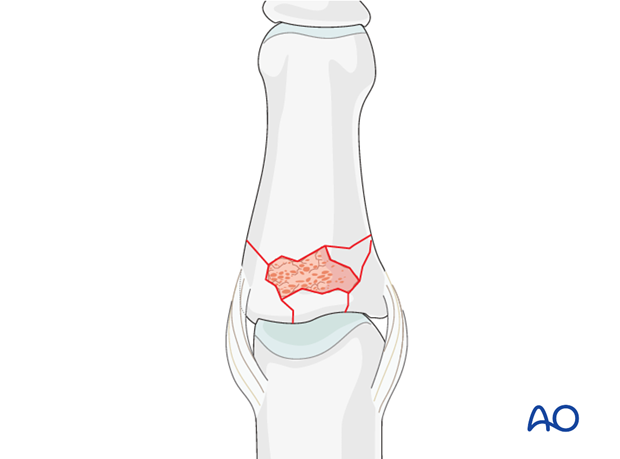
When vertical compression forces, created by axial load, are applied to the finger, comminuted, intraarticular, compression fractures may result. These fractures are very unstable.
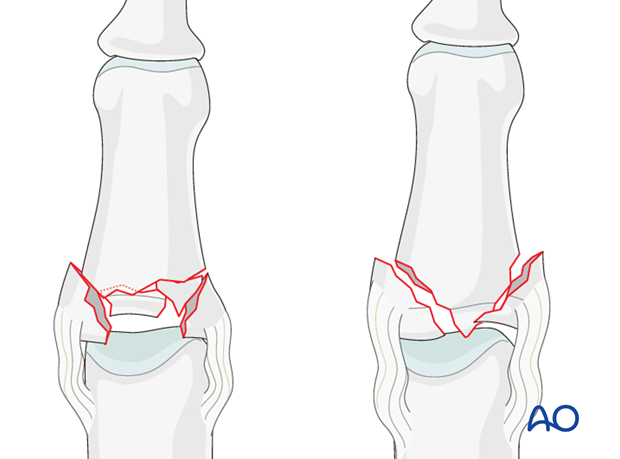
Typically, they occur in two configurations:
- as centrally impacted, comminuted fractures, or
- with a T- or Y-type fracture geometry.
It is desirable to obtain stable fixation to allow early motion and to minimize the risk of degenerative joint disease.
2. Approach
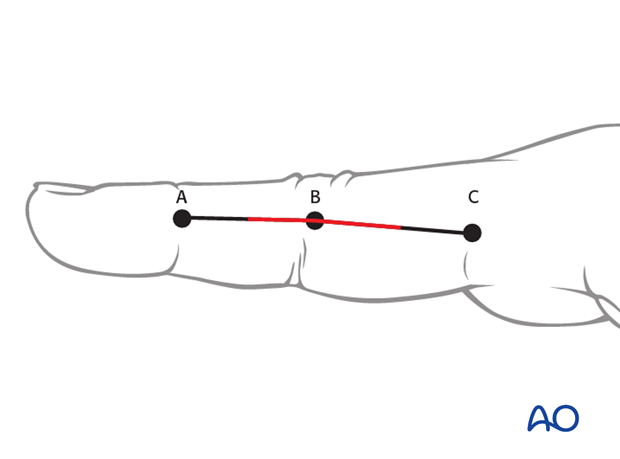
For this procedure a midaxial approach to the PIP joint is normally used.
3. Reduction
Compression fractures are not reducible by ligamentotaxis, as the centrally impacted fragments are devoid of soft-tissue attachments.
Direct reduction is therefore necessary.
The key to fixing compression fractures is restoring the joint surface to as close to normal as possible, and supporting the reduction with bone graft and internal fixation.
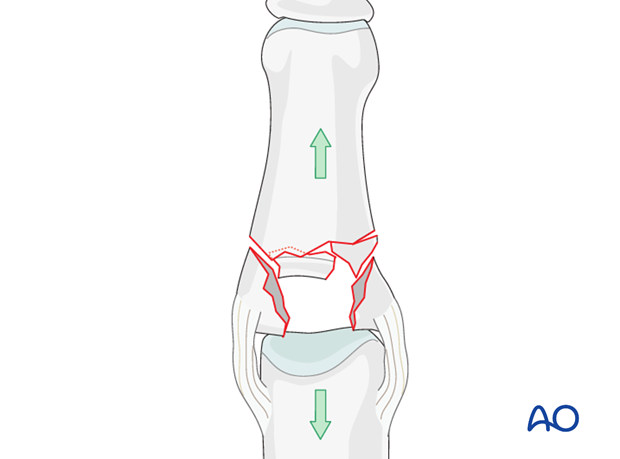
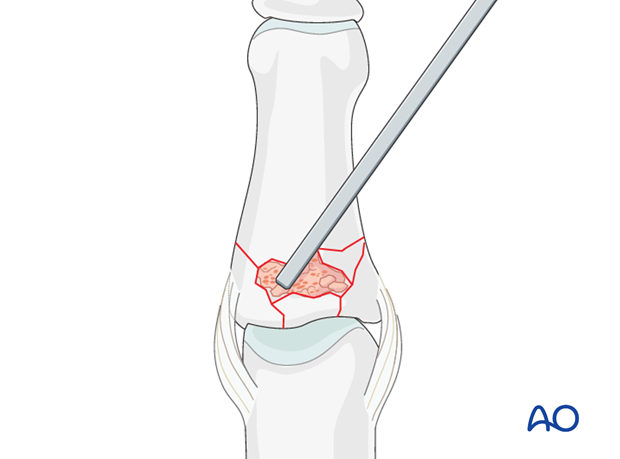
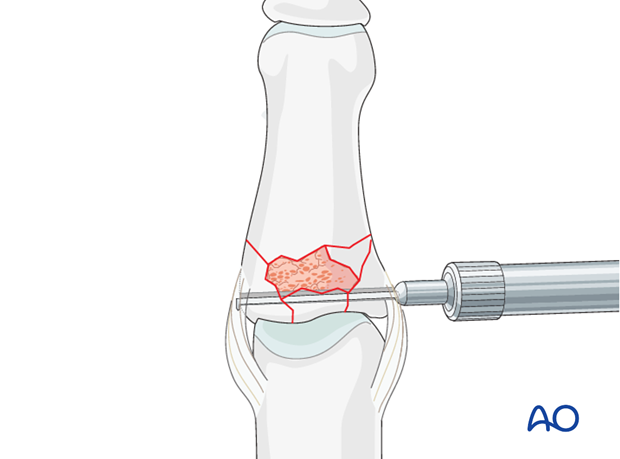
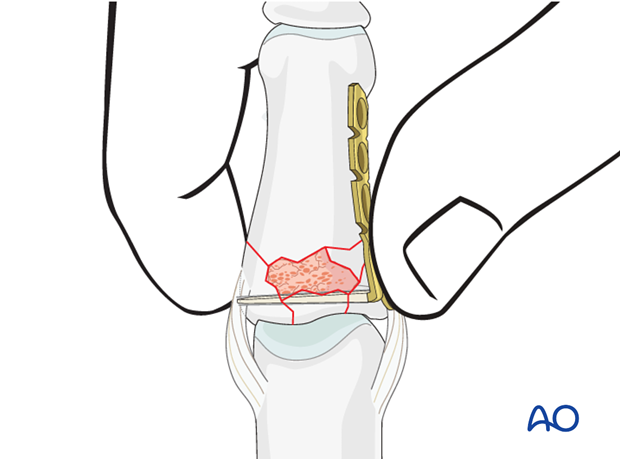
Disimpact the fragments
Using a K-wire, or dental pick, the fragments are disimpacted and pushed towards the head of the metacarpal, which is used as a template to ensure congruity of the articular surface of the phalanx.
If a cartilage step-off greater than 1 mm remains, degenerative joint disease may follow.
Since the metaphyseal cancellous bone is impacted, a void may be created by its disimpaction.
This jeopardizes the fracture in two ways:
- this is a very unstable situation in which the fragments may easily redisplace (collapse)
- the healing process is delayed.
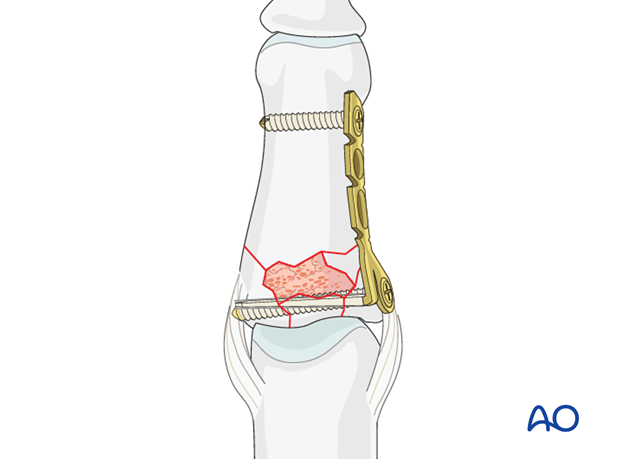
4. Bone graft
Cancellous autograft will be necessary to support the articular fragments and fill the impaction void. The graft will also enhance the healing process.
Preparation of the bone graft
Cancellous bone is harvested from the distal radius or the iliac crest. It is then chopped into tiny pieces and filled into a syringe.

Impact the bone graft
Impact the bone graft using a mallet to compress the syringe plunger. This results in a high concentration of bone cells, increasing the potential for bone regeneration and healing.
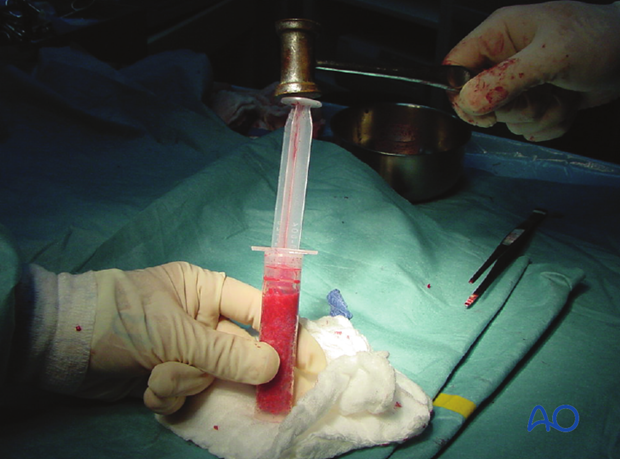
Insert graft into cavity
The bottom of the syringe is cut off using a scalpel.
Insert the compacted bone graft into the cavity by pressure on the plunger.

Using a blunt dissector, impact the bone graft and fill the whole fracture cavity.
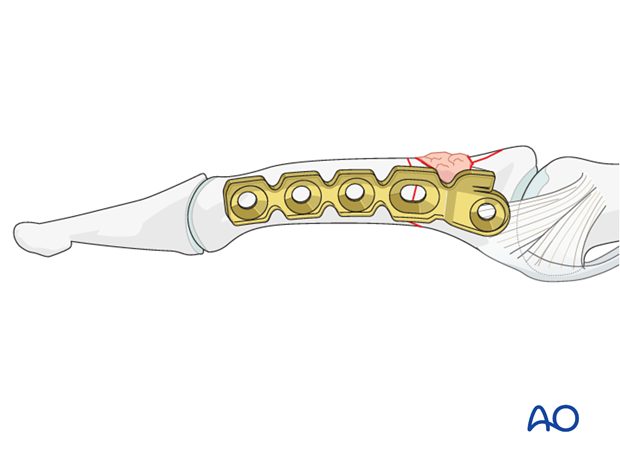
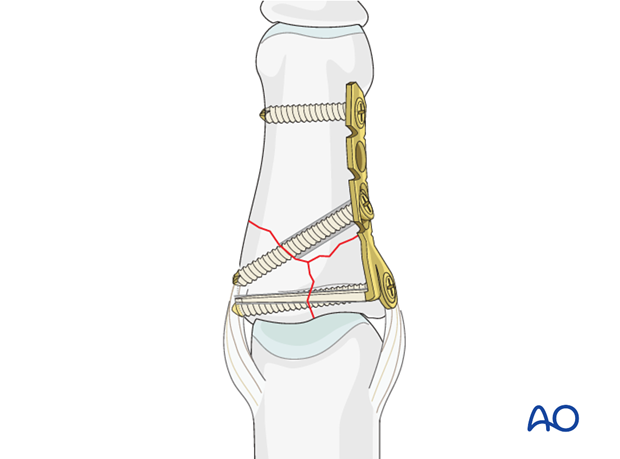
5. Minicondylar plate fixation
Plate selection
Three types of plate are available for treatment of this fracture:
- 1.5 Minicondylar plate
- 1.3 or 1.5 L-plate (adaption plate)
- T-plate
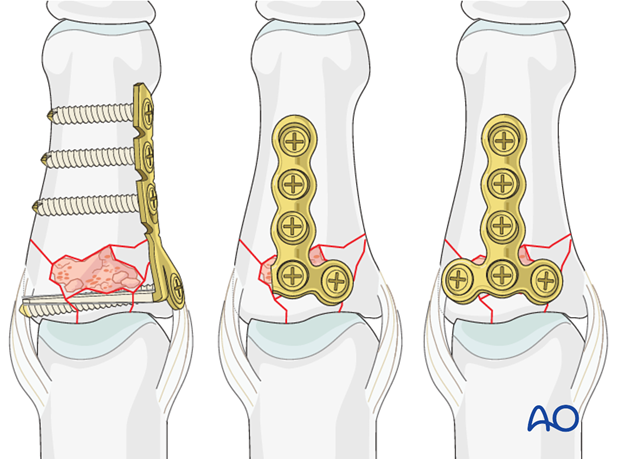
Select a plate according to fragment size, fracture geometry, and surgeon‘s preference.
In the following procedure, only the minicondylar plate fixation will be described. The L-plate is another option, subject to the surgeon’s pereference.
The minicondylar blade plates are available in two forms. One fits on the ulnar aspect of the bone, and the other on the radial aspect. It is a common mistake to choose the wrong one. The correct implant will have the blade dorsal and the distal screw hole palmar.
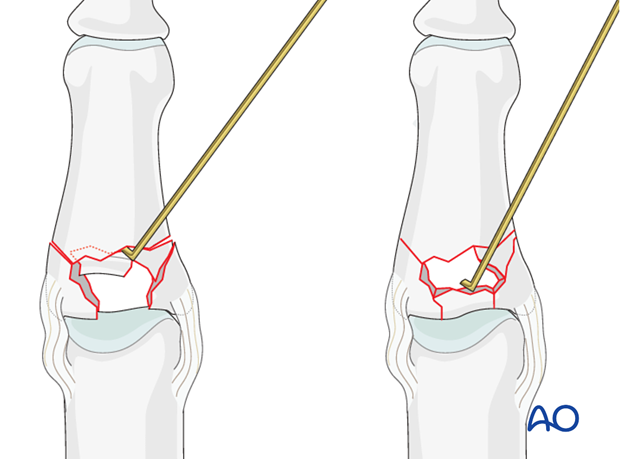
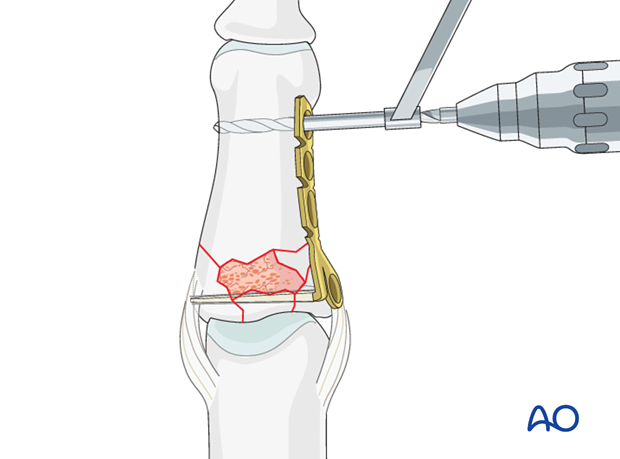
Drilling
In order to determine the position of the first drill hole, it can be very helpful to turn the plate over and use it as a template.
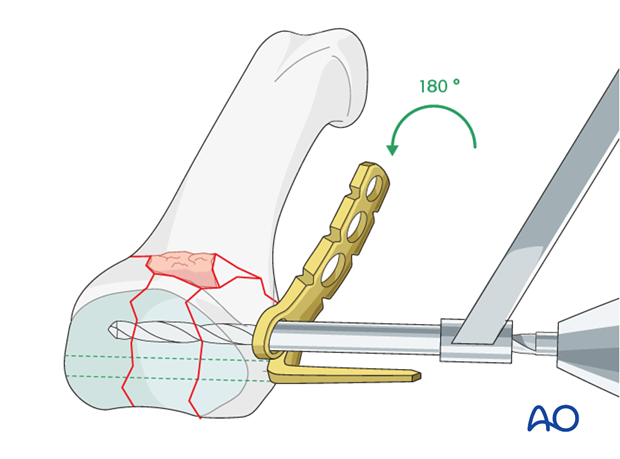
Drill a 1.5 mm transverse hole through the base of the proximal phalanx adjacent to the joint surface as a track for the blade of the plate.
The drill hole needs to be dorsal enough as to leave enough space for the plate’s most proximal screw hole.
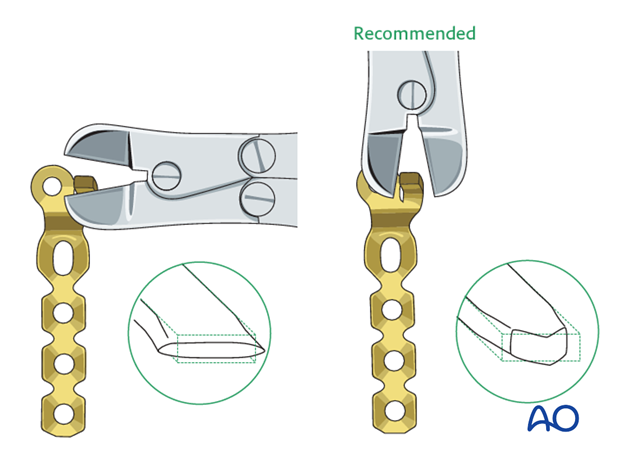
Prepare the blade
Measure the length of the drill hole using a measuring device.
Cut the blade to the determined length, so that it just fills the drill hole.
Pitfall
Avoid protrusion from the opposite cortex, as friction during movement and eventual ligament injury may result.
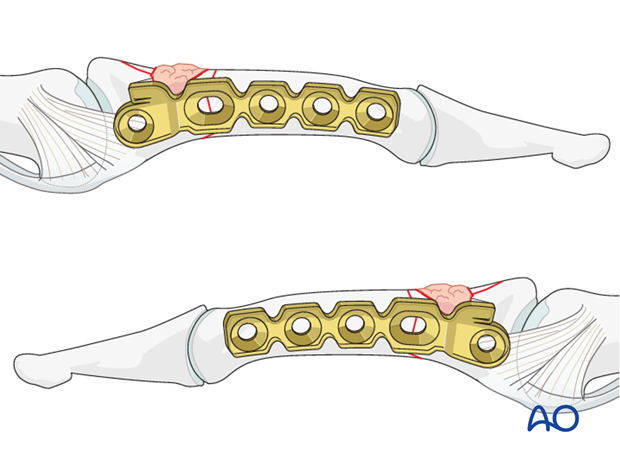
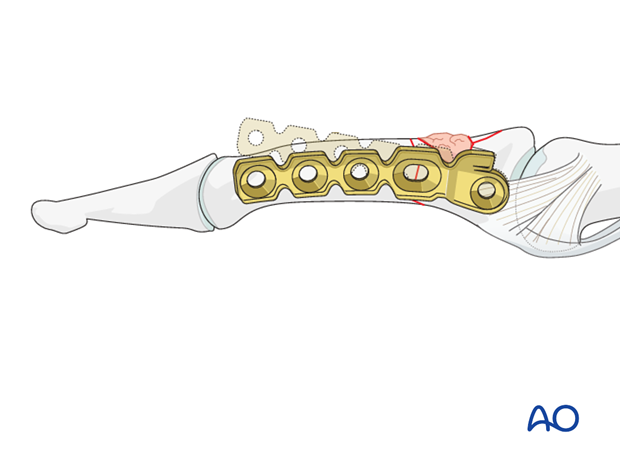
Trim the plate
Adapt the plate length to fit the length of the proximal phalanx. Avoid sharp edges which may be injurious to the tendons. There should be at least 3 plate holes distal to the fracture available for fixation in the diaphysis. At least two screws need to be inserted into the diaphysis.
Pearl: Cut the blade transversely
If you cut the blade on the flat, it will compress and widen very slightly as it is cut. This makes its maximal width very slightly larger than 1.5 mm. It may not fit in the 1.5 mm hole that you have drilled.
Therefore, cut the blade on edge (to deform it through its narrower dimension) to the correct length. The resultant tip is somewhat arrow-shaped.
Contouring of the plate
Use pliers to contour the plate so that it fits exactly the anatomy of the base of the proximal phalanx.
The plate was designed for condylar fractures and is precontoured to fit around a condyle. It has to be adapted for the less curved shape of the base of the proximal phalanx.
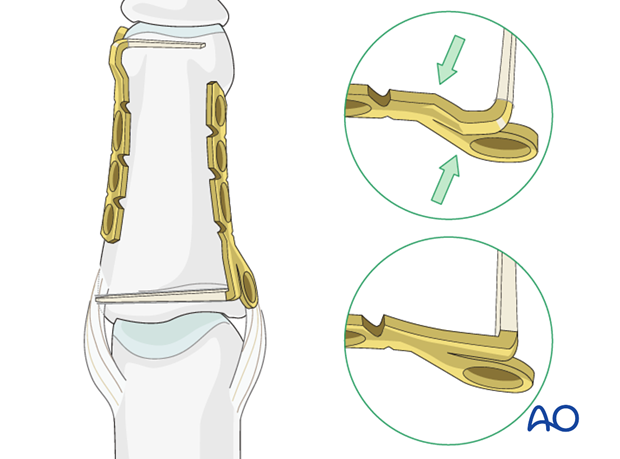
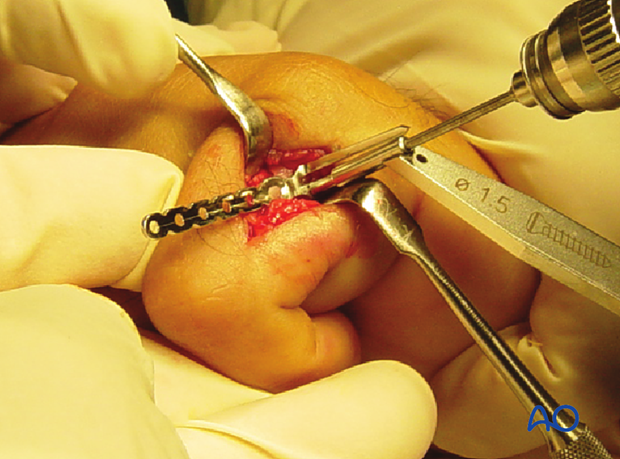
Plate application
Introduce the blade into the drill hole. Gently push with the thumb until the plate is fully seated.
Align the plate with the diaphysis
Before inserting the first (distal) screw, ensure that the plate is in line with the phalangeal diaphysis in the sagittal plane by rotating it around the axis of the blade.
Drill distal hole
Use a 1.1 mm drill bit to prepare the first neutral screw hole at the distal end of the plate.
Insert screw
Measure for screw length and insert a self-tapping 1.5 mm screw.
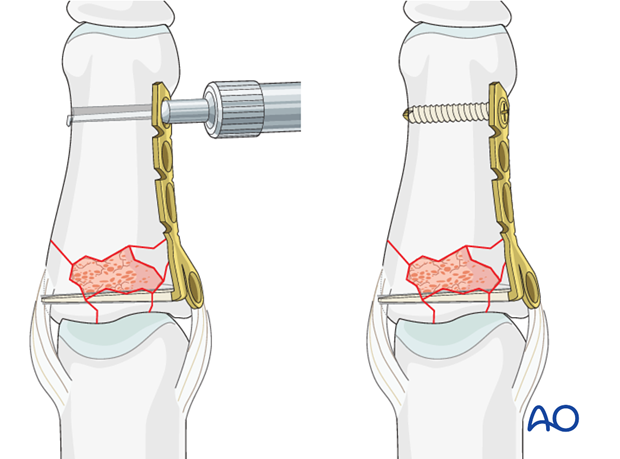
Insert proximal screw
The proximal screw is inserted next, in the same fashion.
The screws should just engage the far cortex. This proximal screw functions as a position screw only.
Do not exert compression through this screw, as this may compromise the reduction of the comminuted zone.
Note
Be careful to avoid protrusion of the proximal screw through the far (trans) cortex, as ligament injury may result from friction during movement.
Fixation of T- or Y-shaped fractures
In these fractures without small-fragment comminution, compression may be employed. Use the proximal screw as a lag screw, and, if possible, insert another lag screw through the oblong plate hole to achieve interfragmentary compression and improve the fixation.
Follow the standard lag screw technique.
Insert a further screw into one of the diaphyseal holes in a neutral position.
6. Aftertreatment
Postoperatively
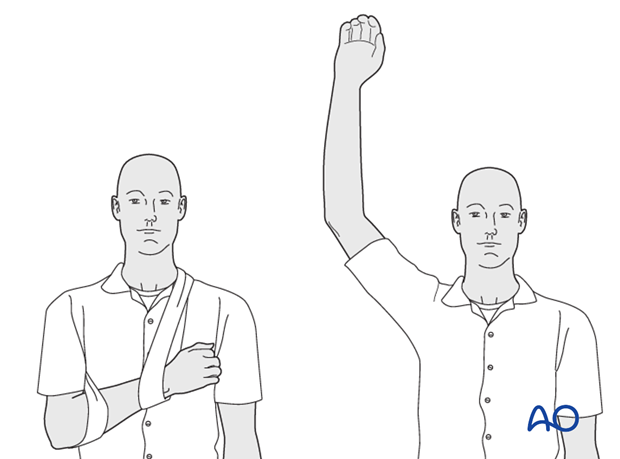
While the patient is in bed, use pillows to keep the hand elevated above the level of the heart to reduce swelling.
Postoperative splint
A removable splint may be applied at the end of the operation, with the hand in an intrinsic plus position (“safe” or “Edinburgh” position).
Immobilize the hand in a safe position for at least 3 weeks.
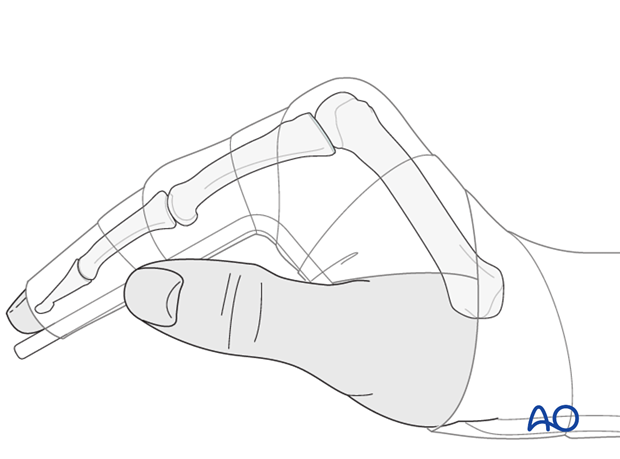
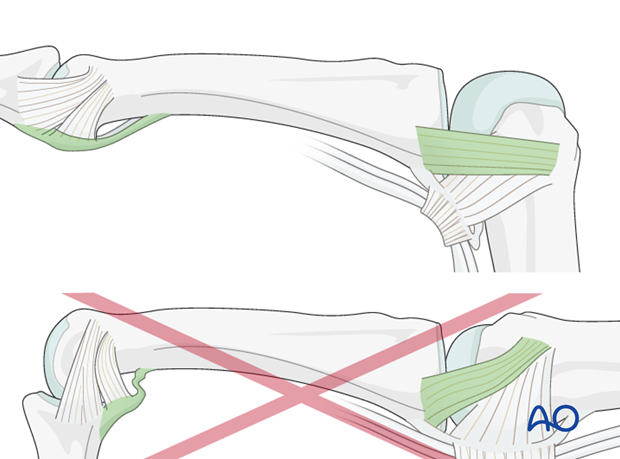
Keep ligament extended
The reason of immobilization of the MCP joint in flexion is to maintain its collateral ligament at maximal length, avoiding scar contraction.
PIP joint extension in this position also maintains length of the volar plate.
Pitfall: scarring
If the collateral ligament develops scarring when not out to length, full extension will become impossible.
Similarly, immobilizing the PIP joint in flexion, can result in scar contraction of the volar plate, also limiting joint extension.
Follow up
See patient 5 days after surgery to check the wound, clean and change the dressing. After 10 days, remove the sutures. Check x-rays.
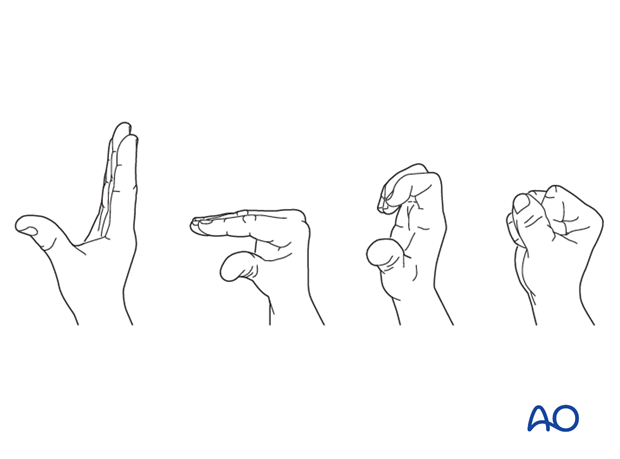
Functional exercises
The fixation will be vulnerable for the first 3-4 weeks.
At this stage, remove the splint, and apply buddy strapping.
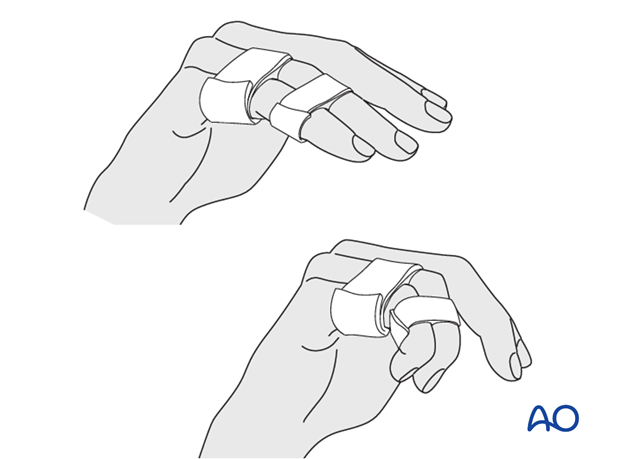
Then begin with active motion exercises.
Instruct the patient to lift the hand regularly overhead, in order to mobilize the shoulder and elbow joints.
Implant removal
The implants may need to be removed in cases of soft-tissue irritation.
In case of joint stiffness, or tendon adhesion’s restricting finger movement, tenolysis, or arthrolysis become necessary. In these circumstances, take the opportunity to remove the implants.












