Dorsal approach to the DIP joint
1. Indications
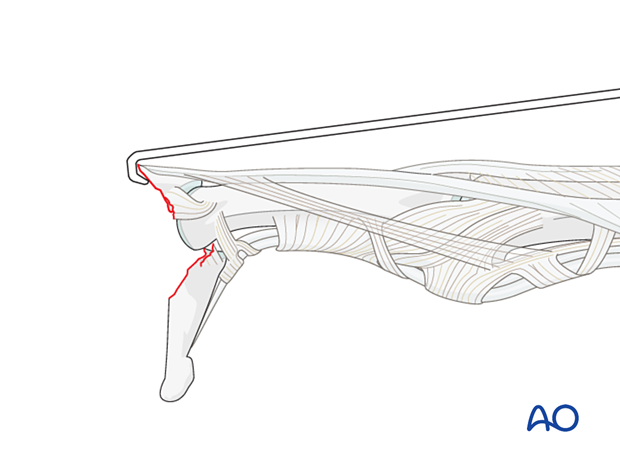
The dorsal approach to the distal interphalangeal (DIP) joint is indicated for extensor tendon avulsion fractures of the dorsal base of the distal phalanx or intraarticular fractures with palmar dislocation.
It is also indicated for DIP arthrodesis.
AO teaching video
Dorsal Approach to Distal Interphalangeal (DIP) Joint of the Finger
2. Surgical anatomy
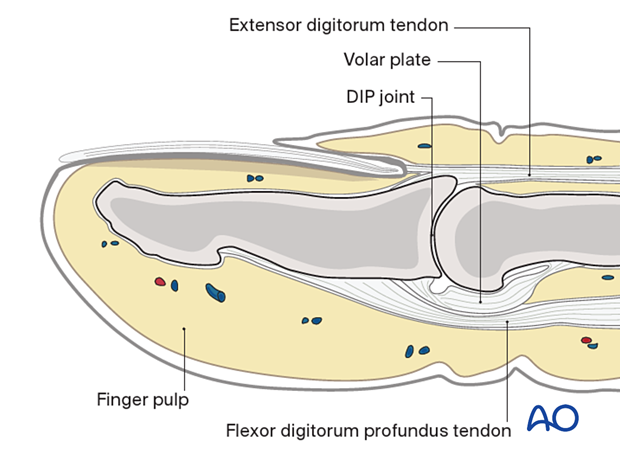
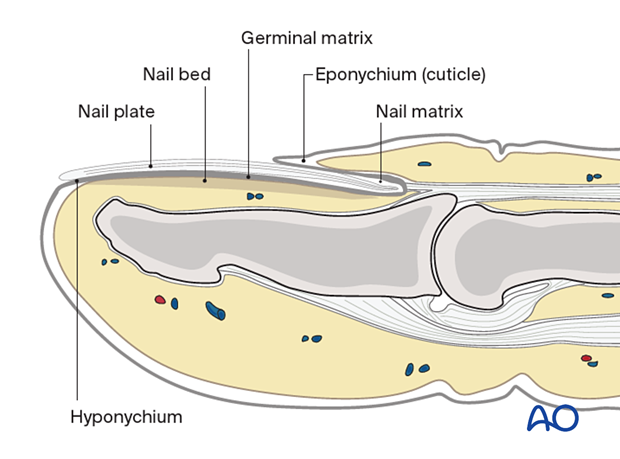
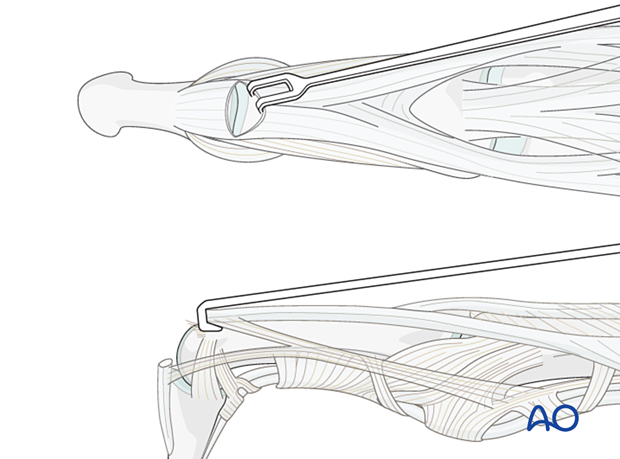
The base of the distal phalanx has a prominent dorsal crest at the insertion of the extensor tendon. The tendon is also adherent to the distal interphalangeal (DIP) joint capsule.
On the palmar surface is the insertion of the flexor digitorum profundus tendon. This is also adherent to the volar plate.
The flexor tendon occupies the whole width of the base of the distal phalanx. It is made up of two different fibers. The superficial fibers attach to the lateral aspects of the phalanx. The deep fibers run centrally and attach more distal in the palmar aspect of the phalanx.
The volar plate is very flexible, allowing hyperextension of the DIP joint and pulp-to-pulp pinch.
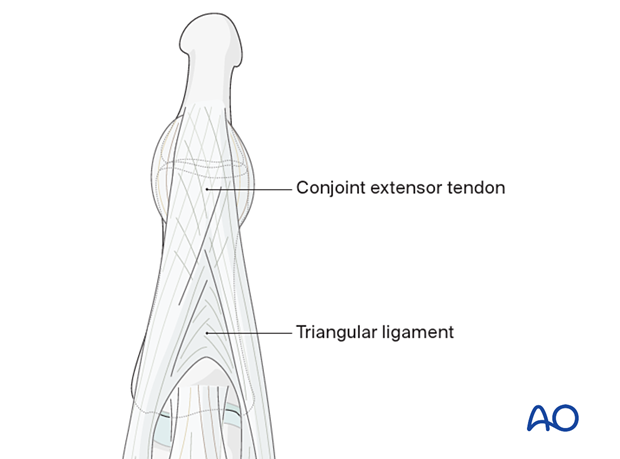
The vascularity of the extensor tendons is more precarious than that of the flexor tendons. This prolongs extensor tendon healing time.
Note the crisscross alignment of the fibers within the conjoint extensor tendons and also within the triangular ligament.
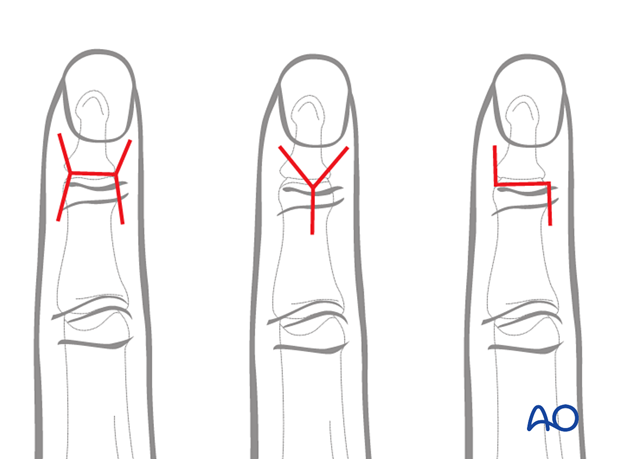
3. Skin incision
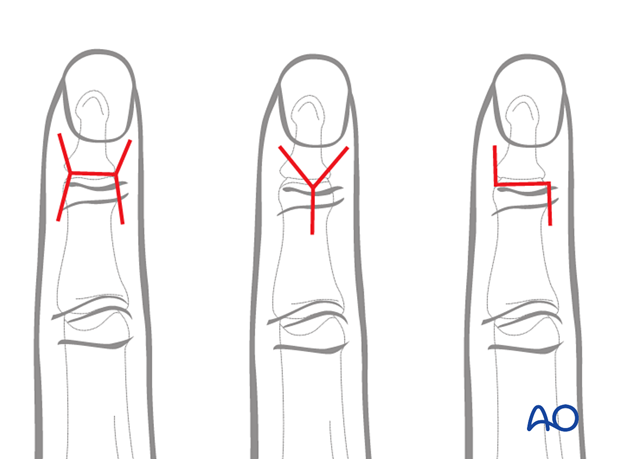
There are three common skin incisions: The H-shaped, the Y-shaped, and the Z-shaped incision.
The H-shaped incision is usually modified by diverging the sides slightly to improve vascularity.
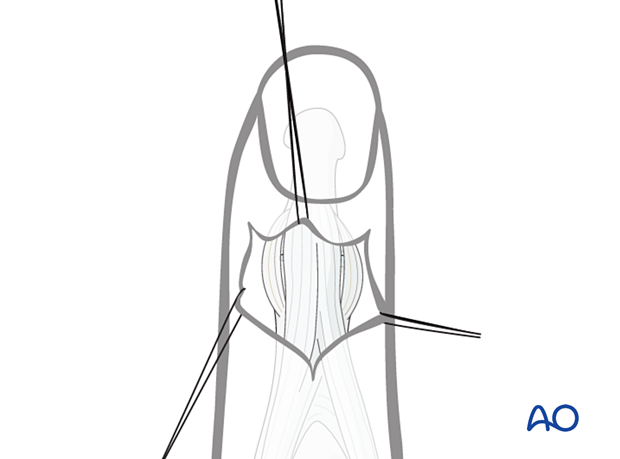
4. Elevation of the skin flaps
Depending on the shape of the skin incision, flaps should be elevated and held with fine sutures to minimize soft-tissue trauma.
Tiny veins will appear and should be coagulated with the bipolar forceps, as necessary, to gain exposure to the joint.
5. Joint exposure
Retract the terminal extensor tendon proximally to expose the DIP joint.
With the collateral ligaments attached to an avulsed fragment, the joint will only be partially visible.
6. Wound closure
Close the skin in a standard manner.












