Lateral paraolecranon approach to the distal humerus
1. General considerations
This is a triceps-on approach that is used primarily for elbow arthroplasty. It can also be used for extraarticular or simple intraarticular distal humeral fractures.
An advantage of this approach is that the triceps insertion remains attached to the ulna. This means there is no need to repair and protect the triceps insertion at the end of the procedure.
A disadvantage is that access to the ulna for total elbow arthroplasty is more challenging.
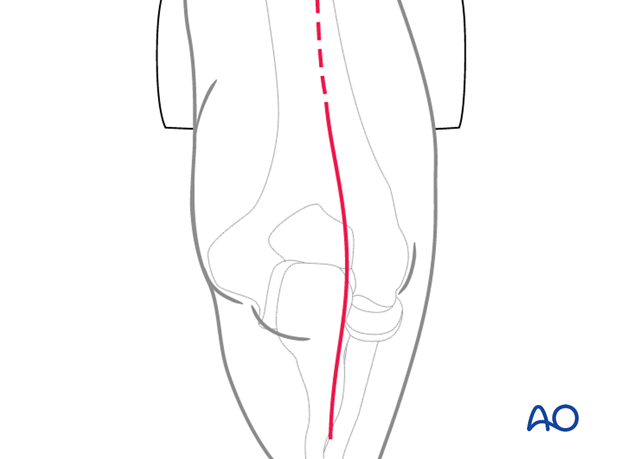
2. Skin incision
Make an incision centered on the junction of the middle and distal thirds of the humeral shaft. Avoid placing the incision over the tip of the olecranon. Some surgeons make a straight incision slightly medial or lateral, whereas others prefer a curved incision. The incision ends over the ulnar diaphysis.
Elevate full-thickness fasciocutaneous flaps to protect the cutaneous nerves.
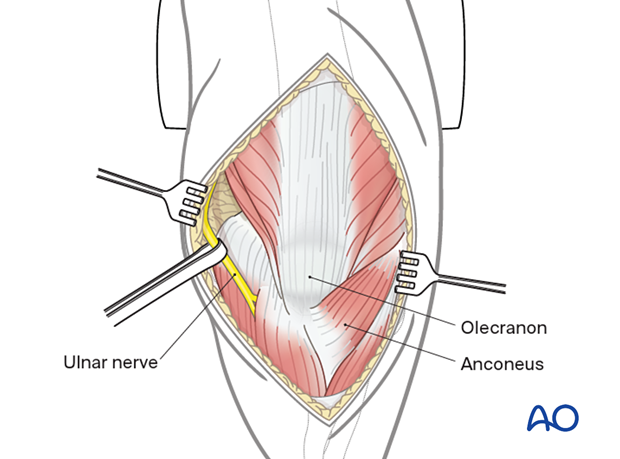
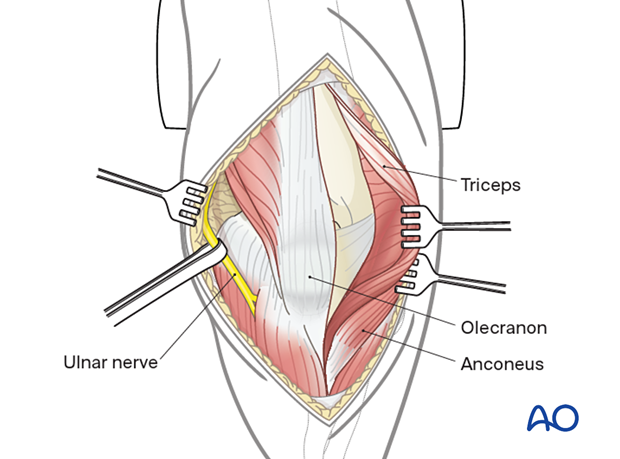
3. Ulnar nerve mobilization
Identify the ulnar nerve proximally along the medial border of the triceps.
Release the ulnar nerve through the cubital tunnel up until the first motor branch by incising the flexor-pronator aponeurosis as the nerve passes between the two heads of flexor carpi ulnaris.
Whenever possible, take care to preserve the perineural vessels.
The nerve may be transposed or left in situ according to the surgeon’s preference, but it should be tension free and not in contact with suture material or metalwork at the end of the procedure.
Take care to protect and be mindful of the nerve throughout the entire procedure.
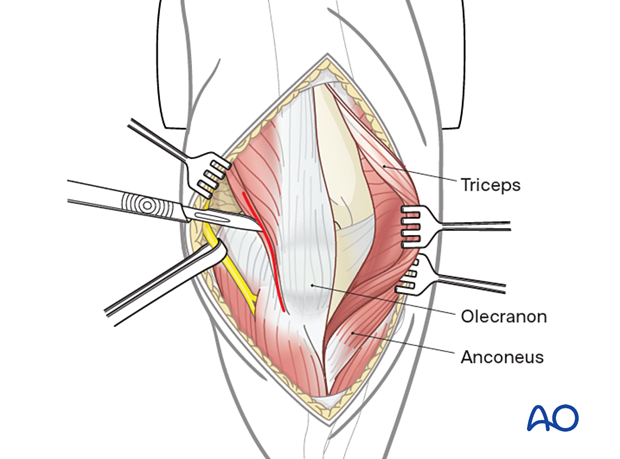
4. Fascial split
Make a split in the anconeus fascia 1 cm lateral to the subcutaneous border of the ulna.
Continue this fascial split proximally lateral to the triceps attachment of the ulna and extend it into the midline of the triceps proximal to the olecranon.
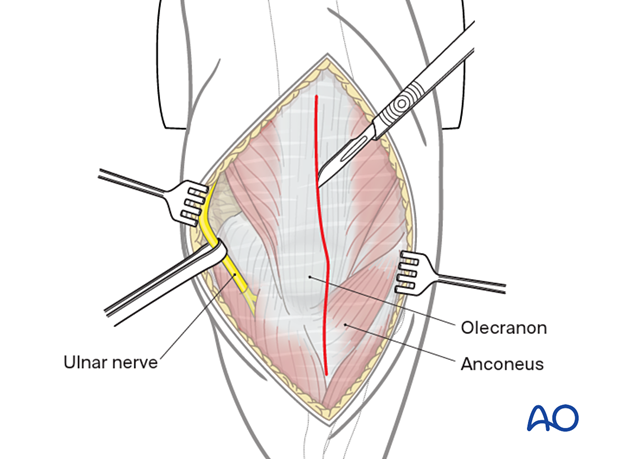
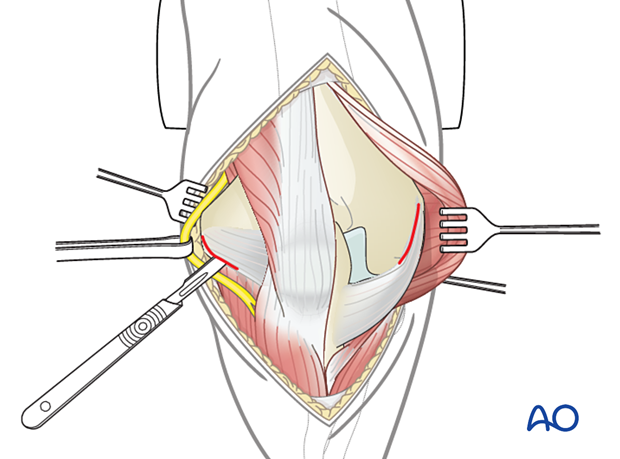
5. Deep dissection
Through the fascial split reflect the anconeus subperiosteally from the lateral aspect of the proximal ulna.
Reflect the anconeus and posterior elbow capsule from the posterior aspect of the lateral column.
Elevate the triceps from the posterior humerus as required.
At this point, because of the more medial split in the triceps compared to a paratricipital approach, it is possible to get a good view of the posterior aspect of the articular surface. Reduction and fixation of the fracture can be performed without an osteotomy.
If further access to the articular surface is required, the approach can easily be converted into an olecranon osteotomy.
For medial plate application, create a further medial window at the medial edge of the triceps as with a paratricipital approach.
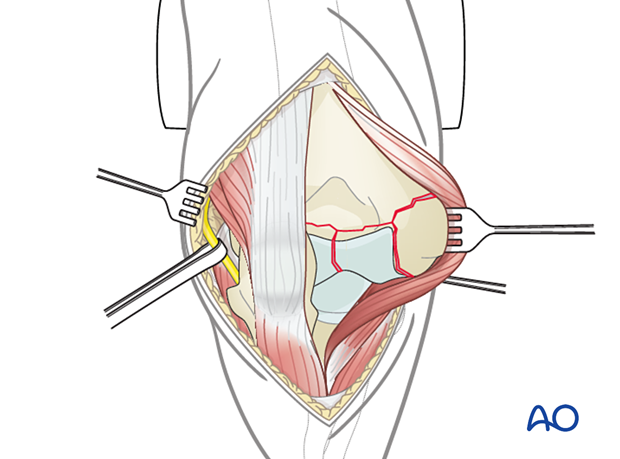
6. Elbow dislocation for arthroplasty
To access the distal humerus, the elbow must be dislocated. In a fracture involving the epicondyles, the humeral shaft can be delivered through the triceps muscle split.
In a fracture not involving the epicondyles, the lateral and medial collateral ligaments must be reflected from the humeral origins to allow dislocation.
The anterior and posterior capsules should be released to allow dislocation.
Dislocated elbow
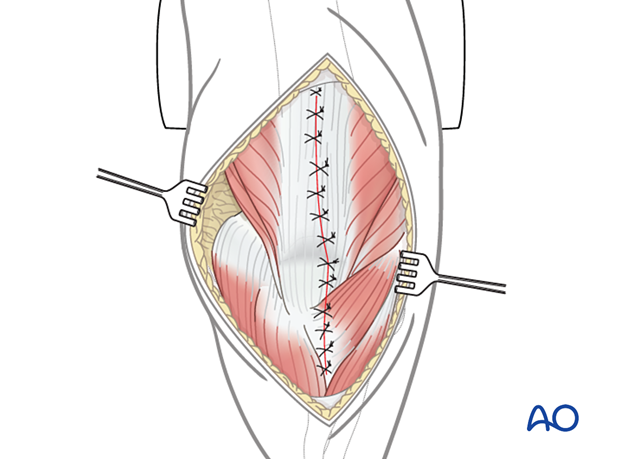
7. Wound closure
Close the wound in layers taking care to repair the medial and lateral collateral ligaments if these have been reflected from the bone.