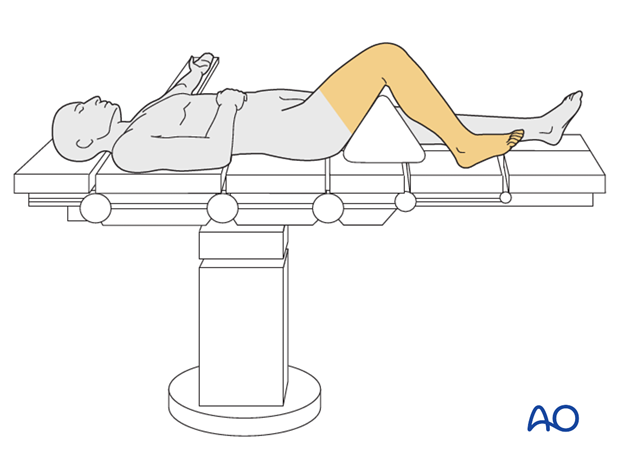
Supine position knee flexed 90°
1. Introduction
This position is useful for plating, nailing, external fixation implementation as the ability to obtain AP and lateral X-rays is exceptional.
Careful pre-cleaning of the soft tissues should be performed especially if gross contamination occurs.
2. Preoperative preparation
- Verify site and side of fracture with the patient along with type of operation planned
- Ensure that operative site has been marked by the surgeon
- Condition of the soft tissues (fracture open or closed)
- Implant to be used (note: plate comes in right and left versions)
- Patient positioning
- Details of the patient (including a signed consent form and appropriate antibiotic and thromboprophylaxis)
- Comorbidities, including allergies
3. Anesthesia
This procedure is performed with the patient under general or regional anesthesia.
If a spinal anesthetic is used, the surgeon and anesthetist need to be confident that the procedure will not last more than 1.5 hours.
Long-lasting postoperative complete pain blocks for the injured leg should be avoided as this could hide symptoms of a subsequent compartment syndrome.
4. Antibiotics
Prophylactic antibiotics
Perioperative antibiotics are required for all distal femoral fractures. The standard first-generation cephalosporin is given at 10 min before surgery and may be given for up to a day after surgery. Antibiotics are administered according to local antibiotic policy and specific patient requirements.
Many surgeons use gram-positive prophylactic antibiotic cover for closed fractures, adding gram-negative prophylactic cover for open fractures.
5. Tourniquet
Tourniquets can be helpful to minimize blood loss and to improve the view of the articular surface. In the trauma patient, the surgeon must consider the effects of ischemia / reperfusion and the potential effects of tourniquet use in the presence of a compromised soft-tissue envelope.
Consideration of tourniquet use should be part of the preoperative planning process. A tourniquet may, or may not, be used depending on the morphology of the fracture and soft-tissue injury. If the fracture margins approach the vicinity of the tourniquet site, a tourniquet is not used.
The surgeon must consider that the inflated tourniquet can complicate the reduction of the fracture by fixing the quadriceps in a shortened position. To avoid this, the knee should be carefully flexed beyond 90° with gentle traction applied and the patella manually pushed distally, in order to gain as much length as possible before the tourniquet is inflated. In some cases, it may be helpful to deflate the tourniquet while reducing the fracture.
A thigh tourniquet should be not left on longer than 120 min., and for a shorter time in older patients or those with known vascular disease.
6. Patient and x-ray positioning
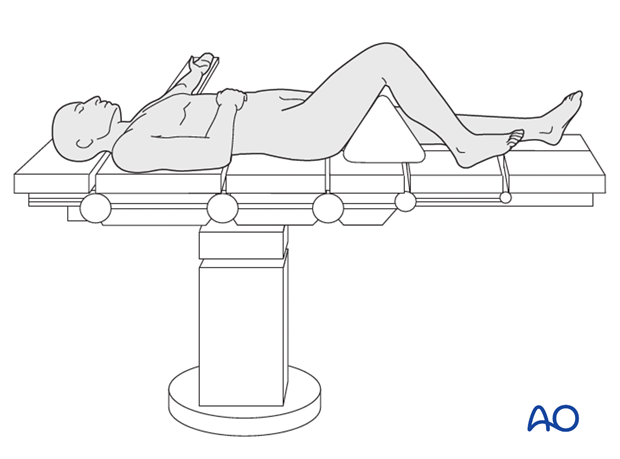
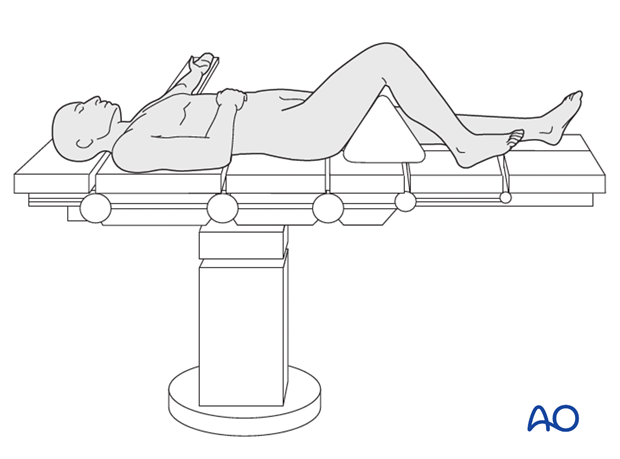
- Place the patient supine on a radiolucent operating table.
- Flexion of the knee up to 90º is required during surgery. This improves visualization of the joint surface and permits the iliotibial band to slip posteriorly from the lateral condyle. Obtain knee flexion either by “breaking” the table at the level of the knee and hanging the lower leg off the end of the table, or using a large bolster under the patient’s thigh
- Place the opposite leg supine on the operating table or into an abducted position with the hip and knee flexed to allow easier access for the image intensifier.
- Ensure that soft tissues, skin pressure points, and the subcutaneous nerves (ulnar nerve at the elbows and peroneal nerve of the opposite knee) are well protected.
- Adjust the operating table to the appropriate height and place the image intensifier on the opposite side of the injury, approaching the knee from the medial aspect.
- Before preparing and draping, ensure adequate imaging of the femur from the hip joint to the knee in the AP and lateral views.
- Carefully pad all pressure points, especially in the elderly.
- Carefully place padding underneath the knee area and proximal fibular region, in order to avoid compression on the popliteal vessels, sciatic nerve and common peroneal nerve. This padding can be easily provided by placing folded towels on the carbon triangle.
- If the fracture is very distal, then a tourniquet may be used. If the has components that are more proximal and fixation goes up above the mid-femur, then the use of tourniquet may not be possible.
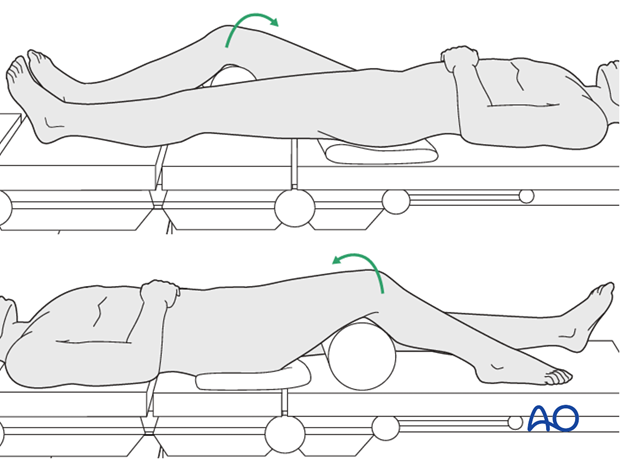
- If the surgeon is approaching the distal femur posterolaterally or posteromedially, then the patient must be prepared so that the limb can be rolled freely from the supine position. If the patient can be rolled either direction, then the surgeon can get direct access to the posteromedial and posterolateral Hoffa fractures. This is done by placing a bolster under the appropriate hip.
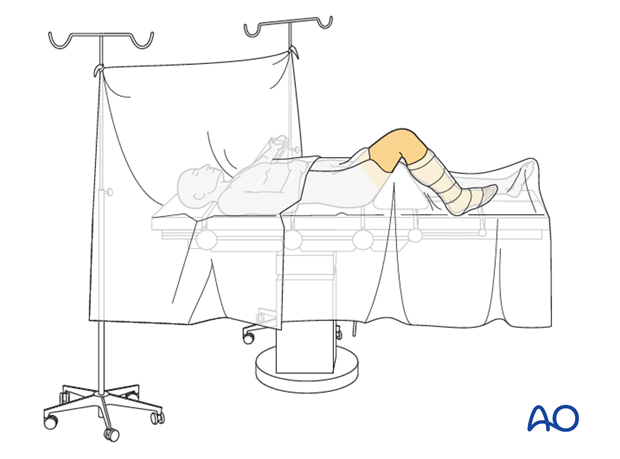
7. Skin disinfecting and draping
Maintain light manual traction (the assistant may need to stand on a stool) on the limb during preparation to avoid excessive deformity at the fracture site.
Disinfect the whole leg from the hip including the foot with the appropriate antiseptic.
- Drape the limb with a single-use U-drape. A stockinette covers the lower leg and is fixed with a tape.
- Drape the leg to allow it to be freely moved.
- Flex the knee to 90° over a bolster.
- Drape the image intensifier.
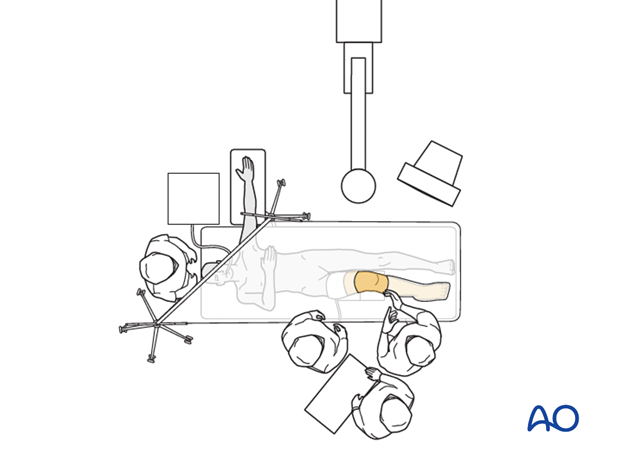
8. Operating room set-up
The surgeon and ORP stand on the side of the affected limb. The assistant stands next to the surgeon.
Place the image intensifier on the opposite side of the injury and the display screen in full view of the surgical team and the radiographer.