Examination of patients with NOE fractures
1. Clinical examination
The patient often has swelling in the medial canthal area and pain and crepitation with palpation.
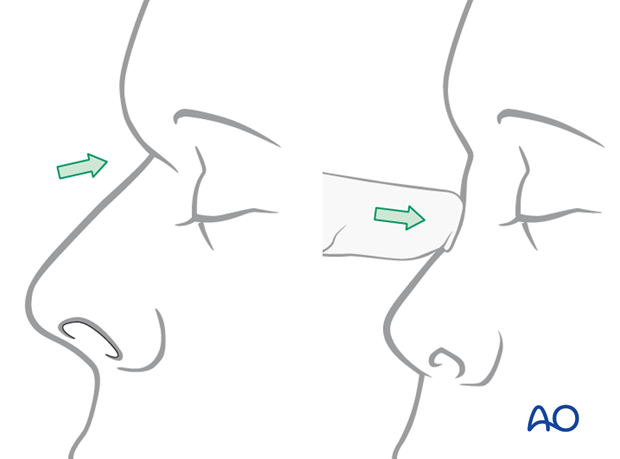
The nose can be retruded and impacted at the nasofrontal suture area with lack of support for the nasal septum and cartilages.
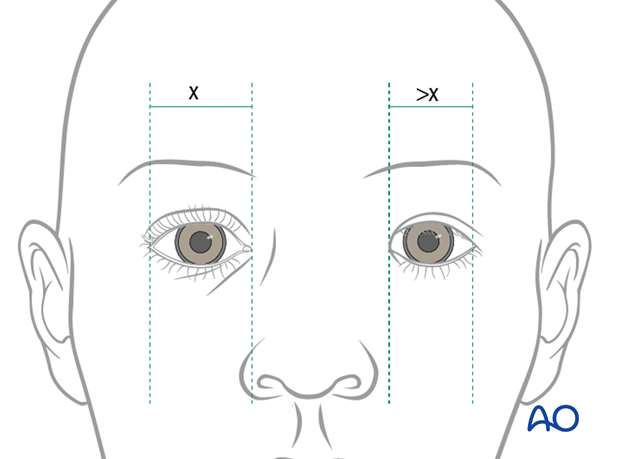
Intercanthal distance
There will be a lack of definition of the bony anatomy in the medial canthal area and possible lateral splaying of the medial canthus with increased intercanthal distance (the normal distance varies depending on the ethnic group, e.g., in Caucasians more than 35 mm intercanthal distance is considered abnormal.)
A thorough ophthalmological examination should be performed.
This illustration demonstrates widening on the left with the medial canthus positioned lateral to the position of the lateral nasal alar margin.
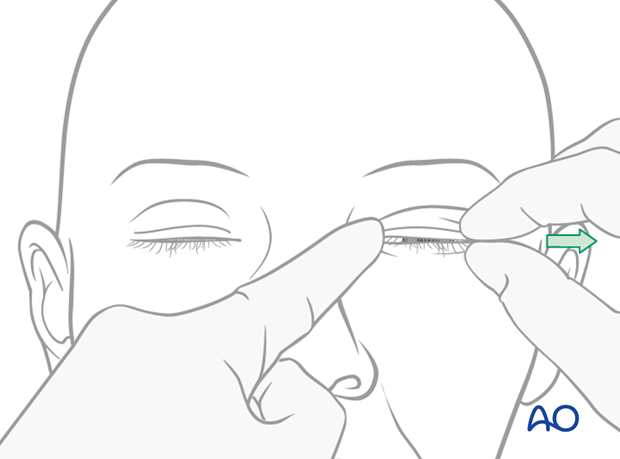
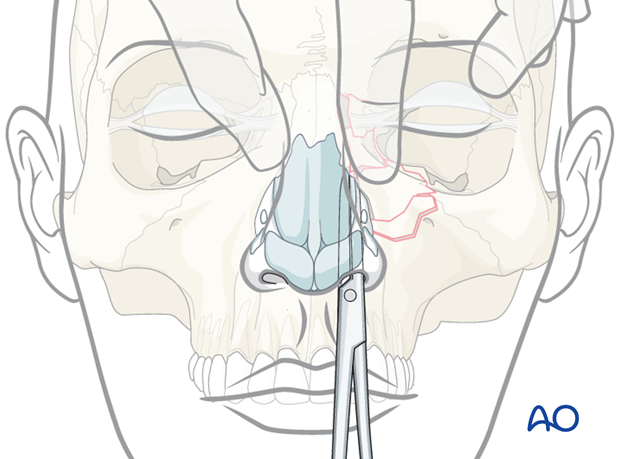
Bow string test
The surgeon may be able to grab the eyelid or use a forceps to grab the skin in the medial canthal area and pull it laterally (“bow-string” test).
In the bow-string test the lid is pulled laterally while the tendon area is palpated to detect movement of fracture segments. A lack of resistance or movement of the underlying bone is indicative of a fracture.
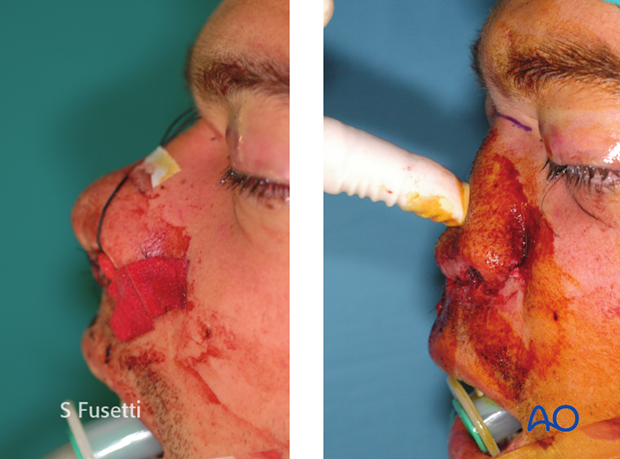
Bimanual palpation
Another test is to place an instrument in the nose and push laterally in the medial canthal area to test for instability and crepitation, which suggests an unstable NOE fracture.
2. Radiographic findings
A surgeon can often distinguish between a type I NOE fracture versus a type II / III fracture by the degree of comminution noted on the CT.
It is generally very difficult to distinguish between a type II and a type III NOE fracture based on radiographic examination. The finding of an avulsed medial canthal tendon from its insertion on the bone often has to be determined intraoperatively.
CT shows a sagittal view of a bilateral NOE type II fracture. Note the depression of the nasal root.
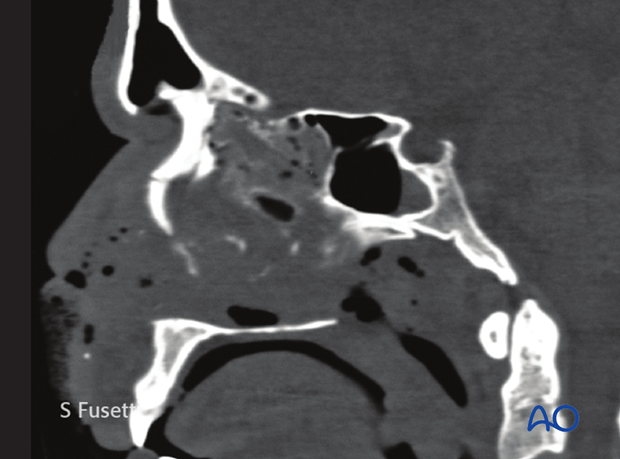
Coronal view of the same patient.
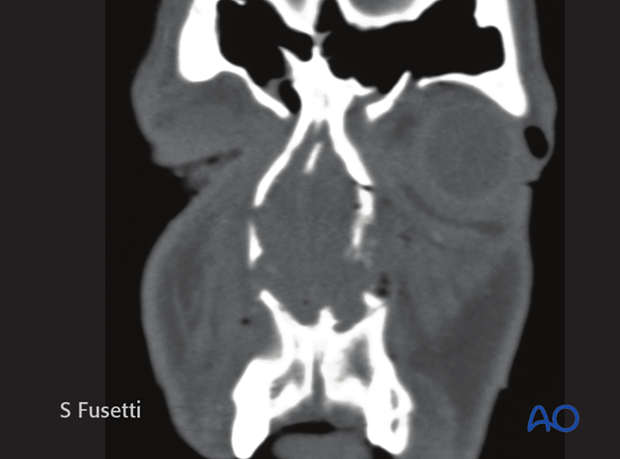
Axial views of the same patient. The axial view shows the involvement and potential compromise of the lacrimal system.
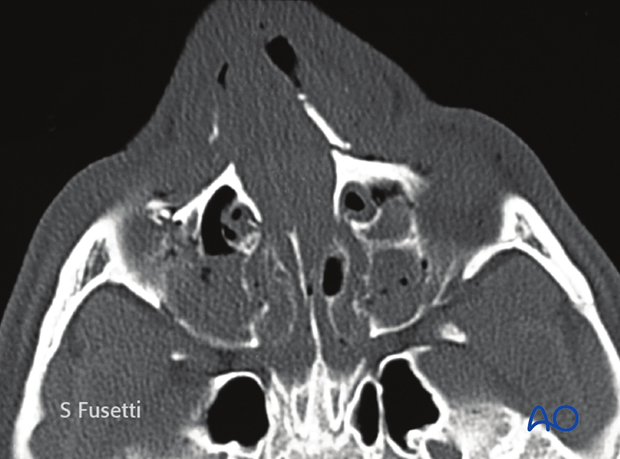
Note the depression of the nasal bone complex.

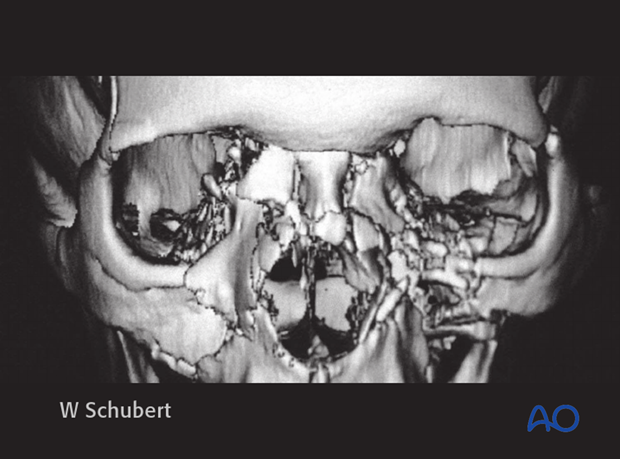
A 3D CT, as shown, can help assessing the severity of the injury but the final diagnosis requires clinical findings and is usually made intraoperatively. This 3D CT shows a bilateral NOE type II with involvement of the nasal bones.
Be aware that a 3D CT often underestimates the severity of the injury.
3. Make sure to rule out CSF leak
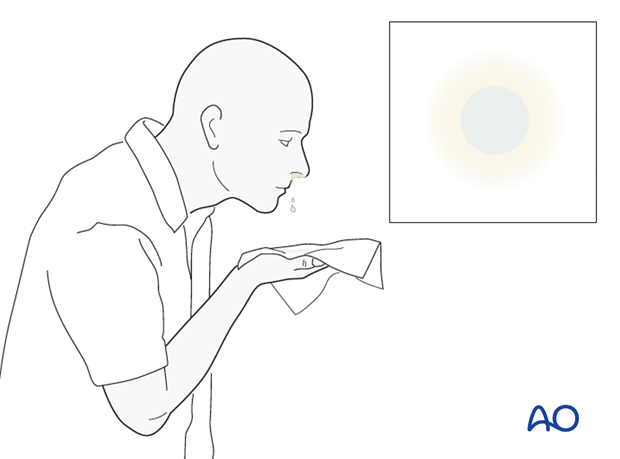
The following diagnostic procedures can be performed if there is a suspected CSF leak (clinical sign: straw-colored or clear nasal drainage):
- Tilt test with positive halo sign (as illustrated)
- CT scan with thin coronal cuts (0.5 mm) of the cribriform plate
- Comparison of the concentration of glucose between fluid and patient’s serum
- Laboratory analysis for beta-transferrin
- Application of fluorescent dyes and direct visualization of the leak via transnasal endoscopy. (Note: in many countries the use of intrathecal dyes is not approved and, therefore, special permission from the patient may be necessary.)
4. Evaluation of lacrimal apparatus
The lacrimal drainage system is intimately related to the NOE region and can be damaged during the trauma. The surgeon should assess the patency/continuity of the nasolacrimal system at the time of surgical treatment.
If there is a discontinuity in the nasolacrimal system repair should be considered at the time of fracture treatment. Click here for a detailed description of repair of the lacrimal system.












