Retromandibular approaches
1. Principles
Introduction
The retromandibular approaches expose the entire ramus from behind the posterior border. Therefore, they are helpful for procedures involving the area on or near the condylar process or the ramus itself.
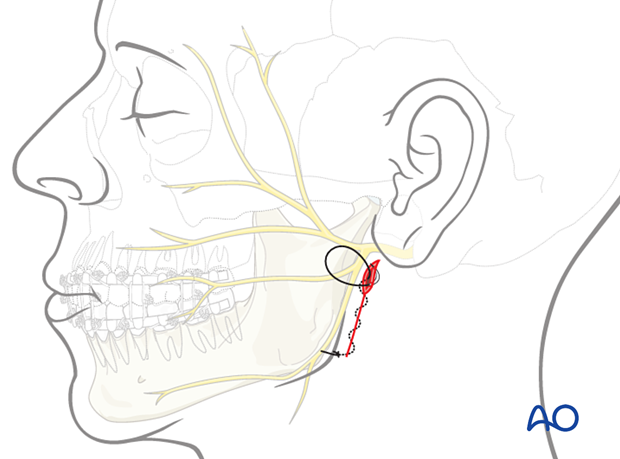
There are two varieties of retromandibular approaches used to access the posterior mandible. They differ in the placement of the incision and the anatomic dissection to the mandible.
- The transparotid approach has the advantage of the close proximity of the skin incision to the area of interest.
- The retroparotid approach has the advantage of not dissecting through the parotid gland.
The facelift (rhytidectomy) approach can be considered as an alternative to retromandibular approaches.
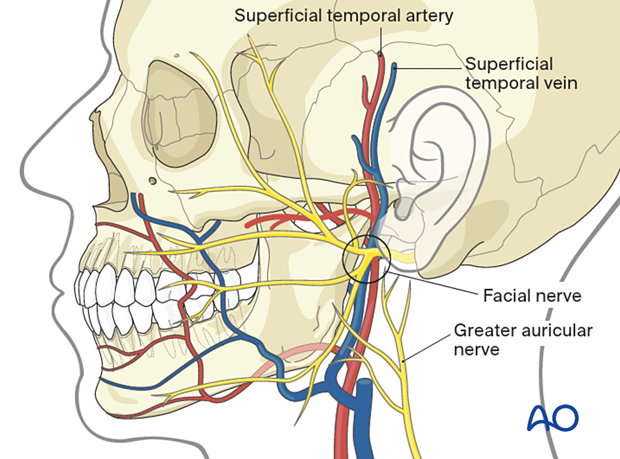
Anatomical structures
The main anatomic structures at risk in these approaches are the main trunk and branches of the facial nerve (CN VII) and the retromandibular vein.
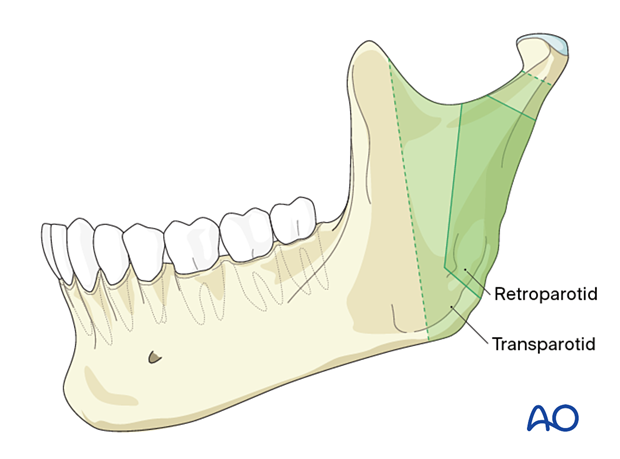
Exposure
The exposure offered by the retromandibular approaches
- Transparotid
- Retroparotid
2. Option 1: Transparotid approach
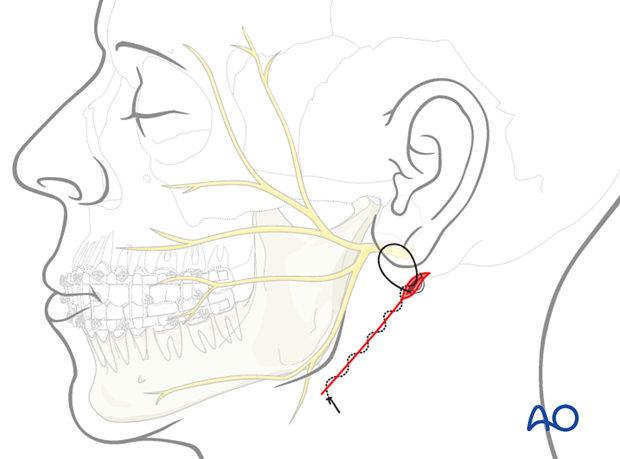
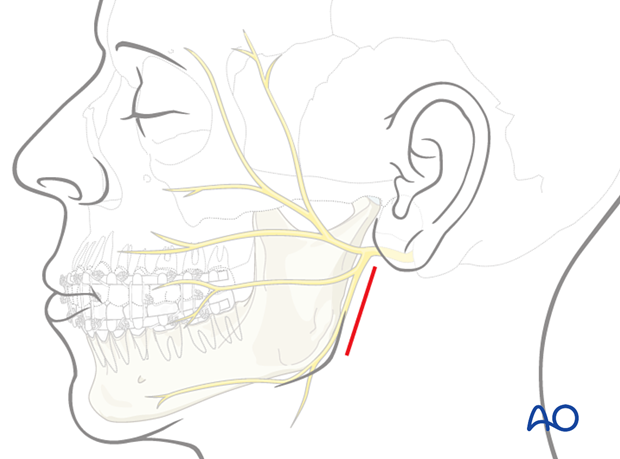
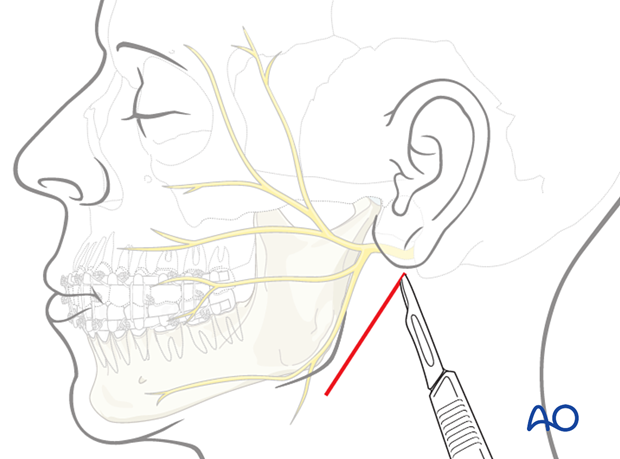
Skin incision
Use of local anesthetic and vasoconstrictorsThe use of a solution containing vasoconstrictors ensures hemostasis at the surgical site. The two options currently available are using a local anesthetic or a physiologic solution with a vasoconstrictor alone.
A local anesthetic with a vasoconstrictor may impair the facial nerve function and impede the use of a nerve stimulator during the surgical procedure. Therefore, consideration should be given to using a physiological solution with a vasoconstrictor alone or injecting the local anesthetic with a vasoconstrictor very superficially.
Muscle relaxants in general anesthesia can also impair nerve function and must be avoided.
A vertical incision through the skin and subcutaneous tissue is made, extending from just below the ear lobe towards the mandibular angle. It should be made parallel to the posterior border of the mandible.
Dissection
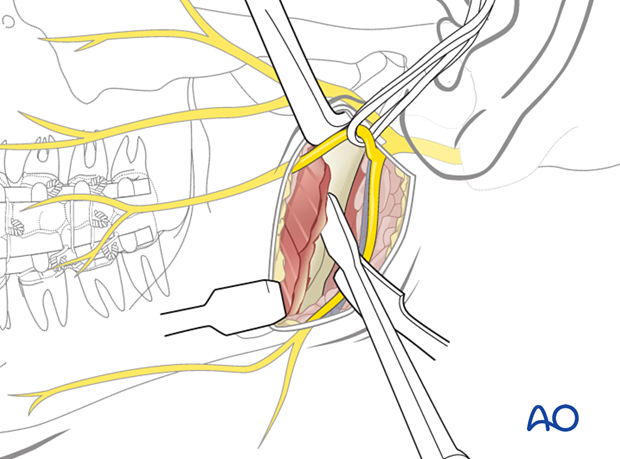
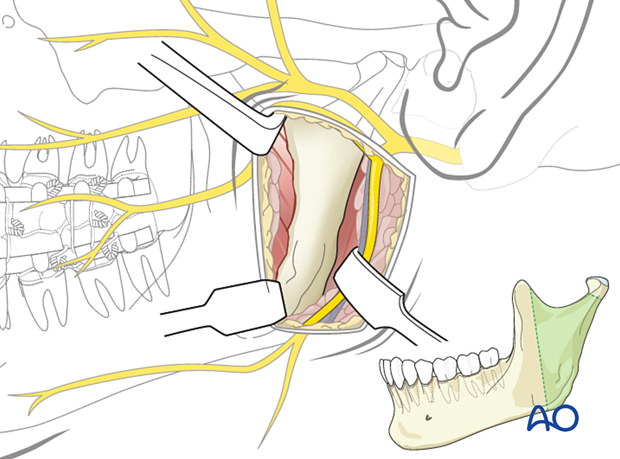
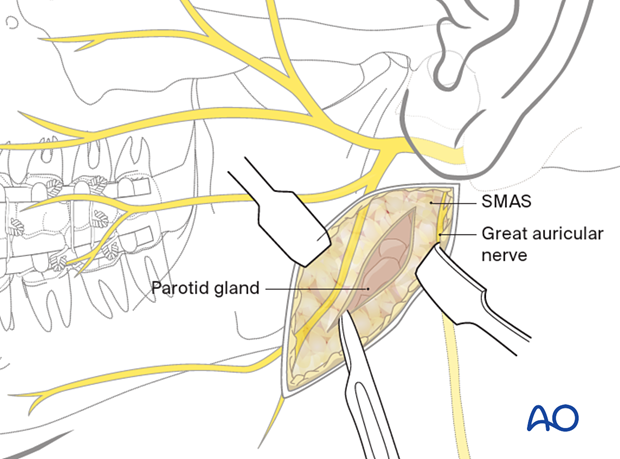
The subcutaneous tissue is undermined, exposing the superficial musculoaponeurotic system (SMAS).
A vertical incision is made through the SMAS into the parotid gland.
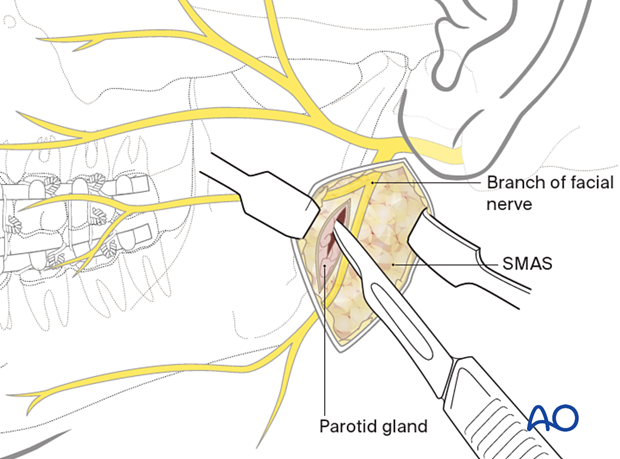
Bluntly dissect the parotid gland parallel to the direction of the facial nerve branches and towards the posterior border of the mandible. The dissection should be anterior to the retromandibular vein.
Branches of the facial nerve may be found during the dissection. A nerve stimulator may be helpful to identify them. They should be identified and protected.
Once the posterior border of the mandible has been reached, an incision is made through the pterygomasseteric sling.
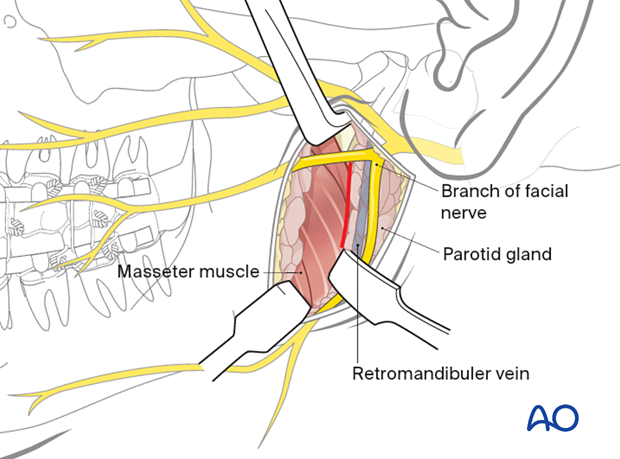
A periosteal elevator is used to strip the masseter muscle from the ramus. Further dissection superiorly along the posterior border exposes the condylar process.
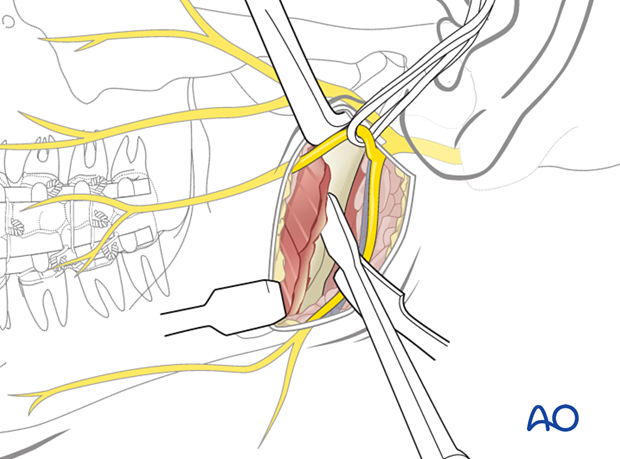
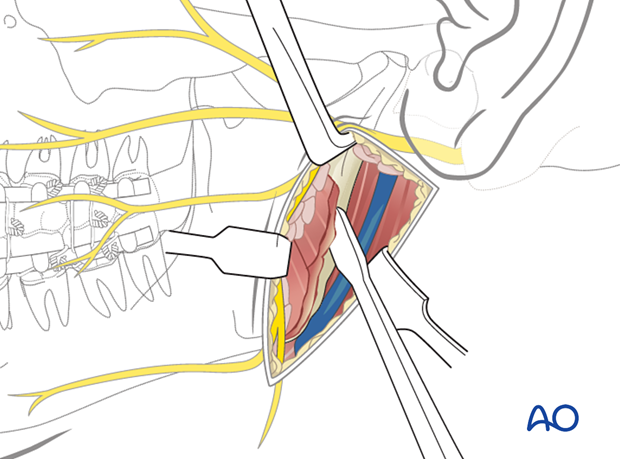
Exposure
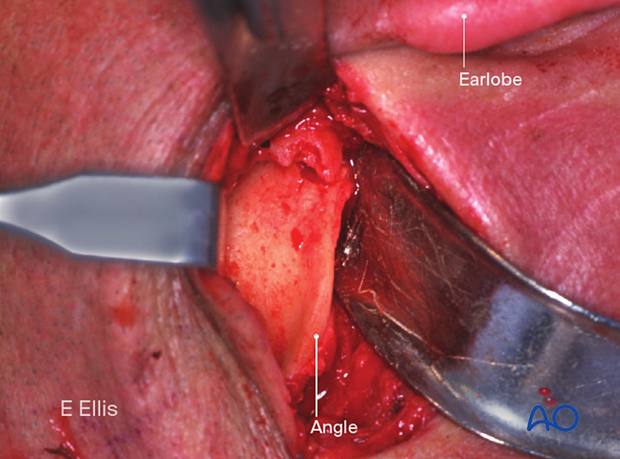
Illustration of the amount of exposure obtained using this approach.
Clinical view of the access gained.
Wound closure
The wound is reapproximated in layers for anatomic realignment and avoidance of dead space. Two sutures are placed through the pterygomasseteric sling (as shown). The parotid gland capsule must be closed tightly to prevent salivary fistula.
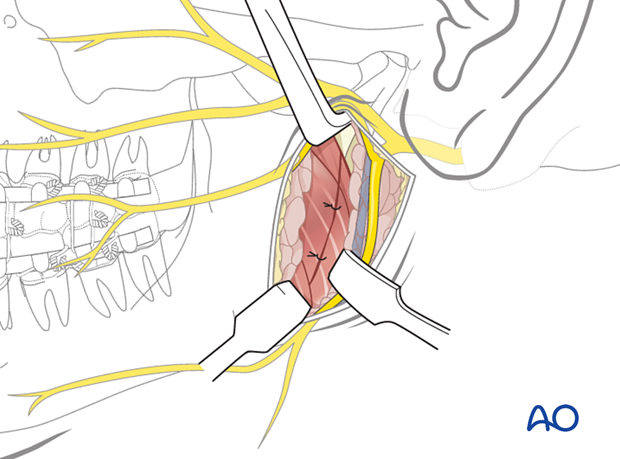
The skin and subcutaneous tissues are then closed based on surgical preference.
Consider anticholinergic medication (transcutaneous patch) postoperatively to decrease salivary flow and lessen the risk of salivary fistula.
3. Option 2: Retroparotid approach
Principles
A frequently used alternative to the retromandibular transparotid approach described above is one in which the parotid gland is lifted rather than dissected through. This requires the incision to be placed more posteriorly, which means that exposure of the mandible is more limited. Rather than approaching the mandible from directly over the ramus, it is approached more posteriorly.
Use of local anesthetic and vasoconstrictorsUse of local anesthetic and vasoconstrictors
The use of a solution containing vasoconstrictors ensures hemostasis at the surgical site. The two options currently available are using a local anesthetic or a physiologic solution with a vasoconstrictor alone.
A local anesthetic with a vasoconstrictor may impair the facial nerve function and impede the use of a nerve stimulator during the surgical procedure. Therefore, consideration should be given to using a physiological solution with a vasoconstrictor alone or injecting the local anesthetic with a vasoconstrictor very superficially.
Muscle relaxants in general anesthesia can also impair nerve function and must be avoided.
Skin incision
An oblique incision through the skin and subcutaneous tissue is made, extending from the mastoid process to a point just below the angle of the mandible.
Dissection
Dissection down to parotid glandThe subcutaneous tissue is undermined, exposing the superficial musculoaponeurotic system (SMAS).
An oblique incision is made through the SMAS. The posterior aspect of the parotid gland is identified, and dissection continues behind the gland.
The gland is lifted off the masseter muscle and retracted anteriorly.
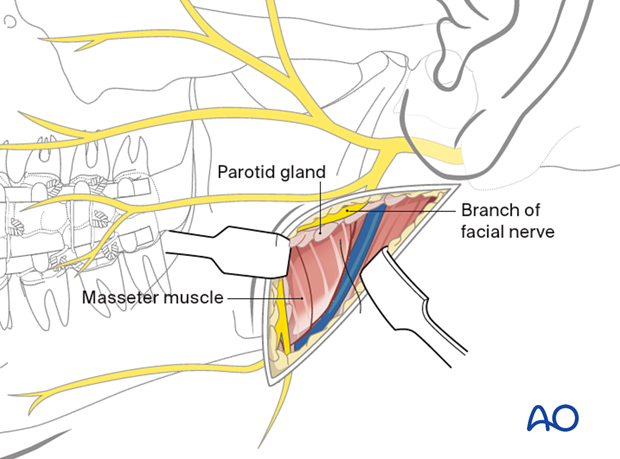
Once the posterior border of the mandible has been reached, an incision is made through the pterygomasseteric sling.
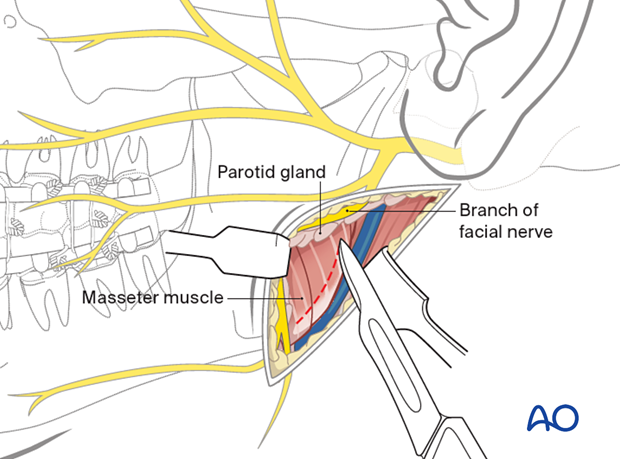
A periosteal elevator is used to strip the masseter muscle from the ramus. Further dissection superiorly along the posterior border exposes the condylar process.
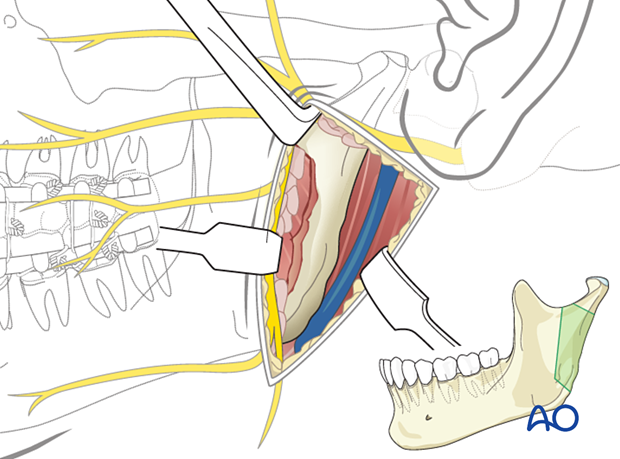
Exposure
Illustration of the amount of exposure obtained using this approach.
Wound closure
The wound is reapproximated in layers for anatomic realignment and avoidance of dead space. Two or three sutures are placed through the pterygomasseteric sling (as shown).
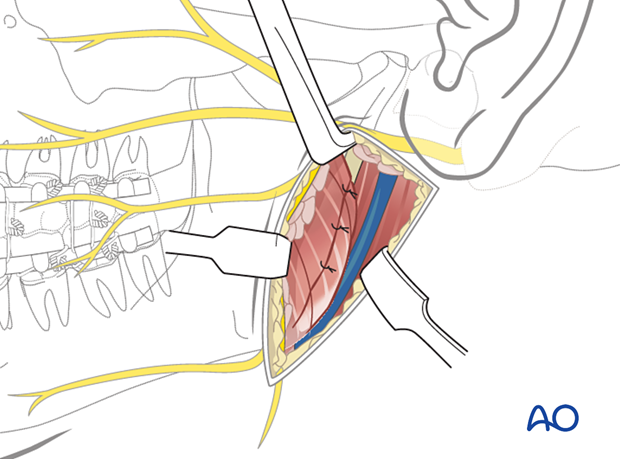
The skin and subcutaneous tissues are then closed based on surgical preference.